Caspofungin 70 Mg Powder For Concentrate For Solution For Infusion
SUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
Caspofungin 70 mg powder for concentrate for solution for infusion
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
Each vial contains 70 mg caspofungin (as acetate).
After reconstitution each ml of the concentrate contains 7.2 mg of caspofungin.
For the full list of excipients, see section 6.1.
3 PHARMACEUTICAL FORM
Powder for concentrate for solution for infusion.
The powder is a white to off-white-compact, powder.
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
- Treatment of invasive candidiasis in adult or paediatric patients.
- Treatment of invasive aspergillosis in adult or paediatric patients who are refractory to or intolerant of amphotericin B, lipid formulations of amphotericin B and/or itraconazole.
Refractoriness is defined as progression of infection or failure to improve after a minimum of 7 days of prior therapeutic doses of effective antifungal therapy.
- Empirical therapy for presumed fungal infections (such as Candida or Aspergillus) in febrile, neutropaenic adult or paediatric patients.
4.2 Posology and method of administration
Caspofungin should be initiated by a physician experienced in the management of invasive fungal infections.
Posology
Adult patients
A single 70 mg loading dose should be administered on Day-1, followed by 50 mg daily thereafter. In patients weighing more than 80 kg, after the initial 70 mg loading dose, caspofungin 70 mg daily is recommended (see section 5.2). No dosage adjustment is necessary based on gender or race (see section 5.2).
Paediatric patients (12 months to 17 years)
In paediatric patients (12 months to 17 years of age), dosing should be based on the patient’s body surface area (see Instructions for Use in Paediatric Patients, Mosteller1 Formula). For all indications, a single 70-mg/m2 loading dose (not to exceed an actual dose of 70 mg) should be administered on Day 1, followed by 50 mg/m2 daily thereafter (not to exceed an actual dose of 70 mg daily). If the 50-mg/m2 daily dose is well tolerated but does not provide an adequate clinical response, the daily dose can be increased to 70 mg/m2 daily (not to exceed an actual daily dose of 70 mg).
The safety and efficacy of caspofungin have not been sufficiently studied in clinical trials involving neonates and infants below 12 months of age. Caution is advised when treating this age group. Limited data suggest that caspofungin at 25 mg/m2 daily in neonates and infants (less than 3 months of age) and 50 mg/m2 daily in young children (3 to 11 months of age) can be considered (see section 5.2).
Duration of treatment
Duration of empirical therapy should be based on the patient’s clinical response. Therapy should be continued until up to 72 hours after resolution of neutropaenia (ANC>500). Patients found to have a fungal infection should be treated for a minimum of 14 days and treatment should continue for at least 7 days after both neutropaenia and clinical symptoms are resolved.
Duration of treatment of invasive candidiasis should be based upon the patient’s clinical and microbiological response. After signs and symptoms of invasive candidiasis have improved and cultures have become negative, a switch to oral antifungal therapy may be considered. In general, antifungal therapy should continue for at least 14 days after the last positive culture.
Duration of treatment of invasive aspergillosis is determined on a case by case basis and should be based upon the severity of the patient’s underlying disease, recovery from immunosuppression, and clinical response. In general, treatment should continue for at least 7 days after resolution of symptoms.
The safety information on treatment durations longer than 4 weeks is limited. However, available data suggest that caspofungin continues to be well tolerated with longer courses of therapy (up to 162 days in adult patients and up to 87 days in paediatric patients).
Special populations
Elderly patients
In elderly patients (65 years of age or more), the area under the curve (AUC) is increased by approximately 30 %. However, no systematic dosage adjustment is required. There is limited treatment experience in patients 65 years of age and older (see section 5.2).
Renal impairment
No dosage adjustment is necessary based on renal impairment (see section 5.2).
Hepatic impairment
For adult patients with mild hepatic impairment (Child-Pugh score 5 to 6), no dosage adjustment is needed. For adult patients with moderate hepatic impairment (Child-Pugh score 7 to 9), caspofungin 35 mg daily is recommended based upon pharmacokinetic data. An initial 70 mg loading dose should be administered on Day-1. There is no clinical experience in adult patients with severe hepatic impairment (Child-Pugh score greater than 9) and in paediatric patients with any degree of hepatic impairment (see section 4.4).
Co-administration with inducers of metabolic enzymes
Limited data suggest that an increase in the daily dose of caspofungin to 70 mg, following the 70 mg loading dose, should be considered when co-administering caspofungin in adult patients with certain inducers of metabolic enzymes (see section 4.5). When caspofungin is co-administered to paediatric patients (12 months to 17 years of age) with these same inducers of metabolic enzymes (see section 4.5), a caspofungin dose of 70-mg/m2 daily (not to exceed an actual daily dose of 70 mg) should be considered.
Method of administration
After reconstitution and dilution, the solution should be administered by slow intravenous infusion over approximately 1 hour.
For instructions on reconstitution of the medicinal product before administration, see section 6.6.
Both 70 mg and 50 mg vials are available.
Caspofungin should be given as a single daily infusion.
4.3 Contraindications
- Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
4.4 Special warnings and precautions for use
Anaphylaxis has been reported during administration of caspofungin. If this occurs, caspofungin should be discontinued and appropriate treatment administered. Possibly histamine-mediated adverse reactions, including rash, facial swelling, angioedema, pruritus, sensation of warmth, or bronchospasm have been reported and may require discontinuation and/or administration of appropriate treatment.
Limited data suggest that less common non-Candida yeasts and non-Aspergillus moulds are not covered by caspofungin. The efficacy of caspofungin against these fungal pathogens has not been established.
Concomitant use of caspofungin with cyclosporin has been evaluated in healthy adult volunteers and in adult patients. Some healthy adult volunteers who received two 3 mg/kg doses of cyclosporin with caspofungin showed transient increases in alanine transaminase (ALT) and aspartate transaminase (AST) of less than or equal to 3-fold the upper limit of normal (ULN) that resolved with discontinuation of the treatment. In a retrospective study of 40 patients treated during marketed use with caspofungin and cyclosporin for 1 to 290 days (median 17.5 days), no serious hepatic adverse reactions were noted. These data suggest that caspofungin can be used in patients receiving cyclosporin when the potential benefit outweighs the potential risk. Close monitoring of liver enzymes should be considered if caspofungin and cyclosporin are used concomitantly.
In adult patients with mild and moderate hepatic impairment, the AUC is increased about 20% and 75 %, respectively. A reduction of the daily dose to 35 mg is recommended for adults with moderate hepatic impairment. There is no clinical experience in adults with severe hepatic impairment or in paediatric patients with any degree of hepatic impairment. A higher exposure than in moderate hepatic impairment is expected and caspofungin should be used with caution in these patients (see sections 4.2 and 5.2).
Laboratory abnormalities in liver function tests have been seen in healthy volunteers and adult and paediatric patients treated with caspofungin. In some adult and paediatric patients with serious underlying conditions who were receiving multiple concomitant medications with caspofungin, cases of clinically significant hepatic dysfunction, hepatitis and hepatic failure have been reported; a causal relationship to caspofungin has not been established. Patients who develop abnormal liver function tests during caspofungin therapy should be monitored for evidence of worsening hepatic function and the risk/benefit of continuing caspofungin therapy should be reevaluated.
Cases of Stevens-Johnson Syndrome (SJS) and toxic epidermal necrolysis (TEN) have been reported after post-marketing use of caspofungin. Caution should apply in patients with history of allergic skin reactions (see section 4.8)
4.5 Interaction with other medicinal products and other forms of interaction
Studies in vitro show that caspofungin is not an inhibitor of any enzyme in the cytochrome P450 (CYP) system. In clinical studies, caspofungin did not induce the CYP3A4 metabolism of other substances. Caspofungin is not a substrate for P-glycoprotein and is a poor substrate for cytochrome P450 enzymes. However, caspofungin has been shown to interact with other medicinal products in pharmacological and clinical studies (see below).
In two clinical studies performed in healthy adult subjects, cyclosporin A (one 4 mg/kg dose or two 3 mg/kg doses 12 hours apart) increased the AUC of caspofungin by approximately 35 %. These AUC increases are probably due to reduced uptake of caspofungin by the liver. Caspofungin did not increase the plasma levels of cyclosporin. There were transient increases in liver ALT and AST of less than or equal to 3-fold the upper limit of normal (ULN) when caspofungin and cyclosporin were co-administered, that resolved with discontinuation of the medicinal products. In a retrospective study of 40 patients treated during marketed use with caspofungin and cyclosporin for 1 to 290 days (median 17.5 days), no serious hepatic adverse reactions were noted (see section 4.4). Close monitoring of liver enzymes should be considered if the two medicinal products are used concomitantly.
Caspofungin reduced the trough concentration of tacrolimus by 26 % in healthy adult volunteers. For patients receiving both therapies, standard monitoring of tacrolimus blood concentrations and appropriate tacrolimus dosage adjustments are mandatory.
Clinical studies in healthy adult volunteers show that the pharmacokinetics of caspofungin are not altered to a clinically relevant extent by itraconazole, amphotericin B, mycophenolate, nelfinavir, or tacrolimus. Caspofungin did not influence the pharmacokinetics of amphotericin B, itraconazole, rifampicin or mycophenolate mofetil. Although safety data are limited it appears that no special precautions are needed when amphotericin B, itraconazole, nelfinavir or mycophenolate mofetil are co-administered with caspofungin.
Rifampicin caused a 60 % increase in AUC and 170 % increase in trough concentration of caspofungin on the first day of co-administration when both medicinal products were initiated together in healthy adult volunteers. Caspofungin trough levels gradually decreased upon repeated administration. After two weeks’ administration rifampicin had limited effect on AUC, but trough levels were 30 % lower than in adult subjects who received caspofungin alone. The mechanism of interaction could possibly be due to an initial inhibition and subsequent induction of transport proteins. A similar effect could be expected for other medicinal products that induce metabolic enzymes. Limited data from population pharmacokinetics studies indicate that concomitant use of caspofungin with the inducers efavirenz, nevirapine, rifampicin, dexamethasone, phenytoin, or carbamazepine may result in a decrease in caspofungin AUC. When co-administering inducers of metabolic enzymes, an increase in the daily dose of caspofungin to 70 mg, following the 70 mg loading dose, should be considered in adult patients (see section 4.2).
All adult drug-drug interaction studies described above were conducted at a 50 or 70 mg daily caspofungin dose. The interaction of higher doses of caspofungin with other medicinal products has not been formally studied.
In paediatric patients, results from regression analyses of pharmacokinetic data suggest that co-administration of dexamethasone with caspofungin may result in clinically meaningful reductions in caspofungin trough concentrations. This finding may indicate that paediatric patients will have similar reductions with inducers as seen in adults. When caspofungin is co-administered to paediatric patients (12 months to 17 years of age) with inducers of drug clearance, such as rifampicin, efavirenz, nevirapine, phenytoin, dexamethasone, or carbamazepine, a caspofungin dose of 70-mg/m2 daily (not to exceed an actual daily dose of 70 mg) should be considered.
4.6 Fertility, pregnancy and lactation
Pregnancy
There are no or limited data from the use of caspofungin in pregnant women. Caspofungin should not be used during pregnancy unless clearly necessary. Animal studies have shown developmental toxicity (see section 5.3). Caspofungin has been shown to cross the placental barrier in animal studies.
Breast-feeding
It is unknown whether caspofungin is excreted in human milk. Available pharmacodynamic/
toxicological data in animals have shown excretion of caspofungin in milk. Women receiving caspofungin should not breast-feed.
Fertility
For caspofungin, there were no effects on fertility in studies conducted in male and female rats (see section 5.3). There are no clinical data for caspofungin to assess its impact on fertility.
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed.
4.8 Undesirable effects
Hypersensitivity reactions (anaphylaxis and possibly histamine-mediated adverse reactions) have been reported (see section 4.4).
Also reported in patients with invasive aspergillosis were pulmonary oedema, adult respiratory distress syndrome (ARDS), and radiographic infiltrates.
Adult patients
In clinical studies, 1,865 adult individuals received single or multiple doses of caspofungin:
564 febrile neutropaenic patients (empirical therapy study), 382 patients with invasive candidiasis, 228 patients with invasive aspergillosis, 297 patients with localised Candida infections, and 394 individuals enrolled in Phase I studies. In the empirical therapy study patients had received chemotherapy for malignancy or had undergone hematopoietic stem-cell transplantation (including 39 allogeneic transplantations). In the studies involving patients with documented Candida infections, the majority of the patients with invasive Candida infections had serious underlying medical conditions (e.g., haematologic or other malignancy, recent major surgery, HIV) requiring multiple concomitant medications. Patients in the non-comparative Aspergillus study often had serious predisposing medical conditions (e.g., bone marrow or peripheral stem cell transplants, haematologic malignancy, solid tumours or organ transplants) requiring multiple concomitant medications.
Phlebitis was a commonly reported local injection-site adverse reaction in all patient populations. Other local reactions included erythema, pain/tenderness, itching, discharge, and a burning sensation.
Reported clinical and laboratory abnormalities among all adults treated with caspofungin (total 1,780) were typically mild and rarely led to discontinuation.
Tabulated list of adverse reactions
The following adverse reactions were reported during clinical studies and/or postmarketing use:
[Very common (>1/10), Common (>1/100 to <1/10), Uncommon 1/1,000 to <1/100), Not known (cannot be estimated from the available data)]
Blood and lymphatic system disorders:
Common: haemoglobin decreased, haematocrit decreased, white blood cell count decreased
Uncommon: anaemia, thrombocytopaenia, coagulopathy, leukopaenia, eosinophil count increased, platelet count decreased, platelet count increased, lymphocyte count decreased, white blood cell count increased, neutrophil count decreased
Metabolism and nutrition disorders:
Common: hypokalemia
Uncommon: fluid overload, hypomagnesaemia, anorexia, electrolyte imbalance, hyperglycaemia, hypocalcaemia, metabolic acidosis
Psychiatric disorders
Uncommon: anxiety,disorientation, insomnia
Nervous system disorders:
Common: headache
Uncommon: dizziness, dysgeusia, paraesthesia, somnolence, tremor, hypoaesthesia Eye disorders:
Uncommon: ocular icterus, vision blurred, eyelid oedema, lacrimation increased Cardiac disorders:
Uncommon: palpitations, tachycardia, arrhythmia, atrial fibrillation, cardiac failure congestive
Vascular disorders:
Common: phlebitis
Uncommon: thrombophlebitis, flushing, hot flush, hypertension, hypotension
Respiratory, thoracic and mediastinal disorders:
Common: dyspnoea
Uncommon: nasal congestion, pharyngolaryngeal pain, tachypnoea, bronchospasm, cough, dyspnoea paroxysmal nocturnal, hypoxia, rales, wheezing
Gastrointestinal disorders:
Common: nausea, diarrhoea, vomiting
Uncommon: abdominal pain, abdominal pain upper, dry mouth, dyspepsia, stomach discomfort, abdominal distension, ascites, constipation, dysphagia, flatulence
Hepatobiliary disorders:
Common: elevated liver values (alanine aminotransferase, aspartate aminotranserase, blood alkaline phosphatase, bilirubin conjugated, blood bilirubin)
Uncommon: cholestasis, hepatomegaly, hyperbilirubinaemia, jaundice, hepatic function abnormal, hepatotoxicity, liver disorder, gamma-glutamyltransferase increased
Skin and subcutaneous tissue disorders:
Common: rash, pruritus, erythema, hyperhidrosis
Uncommon: erythema multiforme, rash macular, rash maculo-papular, rash pruritic, urticaria, dermatitis allergic, pruritus generalised, rash erythematous, rash generalised, rash morbilliform, skin lesion
Not known:Toxic epidermal necrolysis and Stevens-Johnson Syndrome (see section 4.4)
Musculoskeletal and connective tissue disorders
Common: arthralgia
Uncommon: back pain, pain in extremity, bone pain, muscular weakness, myalgia
Renal and urinary disorders
Uncommon: renal failure, renal failure acute
General disorders and administration site conditions:
Common: pyrexia, chills, infusion-site pruritus
Uncommon: pain, catheter site pain, fatigue, feeling cold, feeling hot, infusion site erythema, infusion site induration, infusion site pain, infusion site swelling, injection site phlebitis, oedema peripheral, tenderness, chest discomfort, chest pain, face oedema, feeling of body temperature change, induration, infusion site extravasation, infusion site irritation, infusion site phlebitis, infusion site rash, infusion site urticaria, injection site erythema, injection site oedema, injection site pain, injection site swelling, malaise, oedema
Investigations:
Common: blood potassium decreased, blood albumin decreased
Uncommon: blood creatinine increased, red blood cells urine positive, protein total decreased, protein urine present, prothrombin time prolonged, prothrombin time shortened, blood sodium decreased, blood sodium increased, blood calcium decreased, blood calcium increased, blood chloride decreased, blood glucose increased, blood magnesium decreased, blood phosphorus decreased, blood phosphorus increased, blood urea increased, activated partial thromboplastin time prolonged, blood bicarbonate decreased, blood chloride increased, blood potassium increased, blood pressure increased, blood uric acid decreased, blood urine present, breath sounds abnormal, carbon dioxide decreased, immunosuppressant drug level increased, international normalised ratio increased, urinary casts, white blood cells urine positive, and pH urine increased.
Caspofungin has also been evaluated at 150 mg daily (for up to 51 days) in 100 adult patients (see section 5.1). The study compared caspofungin at 50 mg daily (following a 70-mg loading dose on Day 1) versus 150 mg daily in the treatment of invasive candidiasis. In this group of patients, the safety of caspofungin at this higher dose appeared generally similar to patients receiving the 50-mg daily dose of caspofungin. The proportion of patients with a serious drug-related adverse reaction or a drug-related adverse reaction leading to caspofungin discontinuation was comparable in the 2 treatment groups.
Paediatric Patients
Data from 5 clinical studies completed in 171 paediatric patients suggest that the overall incidence of clinical adverse experiences (26.3%; 95% CI -19.9, 33.6) is not worse than reported for adults treated with caspofungin (43.1%; 95% CI -40.0, 46.2). However, paediatric patients probably have a different adverse event profile compared to adult patients. The most common drug-related clinical adverse experiences reported in paediatric patients treated with caspofungin were pyrexia (11.7%), rash (4.7%) and headache (2.9%).
The following adverse reactions were reported:
[Very common feJ/10), Common (>1/100 to <1/10)]
Blood and lymphatic system disorders:
Common: eosinophil count increased
Nervous system disorders:
Common: headache
Cardiac disorders:
Common: tachycardia
Vascular disorders:
Common: flushing, hypotension
Hepatobiliary disorders:
Common: elevated liver enzyme levels (AST, ALT)
Skin and subcutaneous tissue disorders:
Common: rash, pruritus
General disorders and administration site conditions:
Very common: fever Common: chills, catheter site pain
Investigations:
Common: decreased potassium, hypomagnesemia, increased glucose, decreased phosphorus, and increased phosphorus
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
4.9 Overdose
Inadvertent administration of up to 400 mg of caspofungin in one day has been reported. These occurrences did not result in clinically important adverse reactions. Caspofungin is not dialysable.
5 PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: antimycotics for systemic use, ATC Code: J02AX04
Mechanism of action
Caspofungin acetate is a semi-synthetic lipopeptide (echinocandin) compound synthesised from a fermentation product of Glarea lozoyensis. Caspofungin acetate inhibits the synthesis of beta (1,3)-D-glucan, an essential component of the cell wall of many filamentous fungi and yeast.
Beta (1,3)-D-glucan is not present in mammalian cells.
Fungicidal activity with caspofungin has been demonstrated against Candida yeasts. Studies in vitro and in vivo demonstrate that exposure of Aspergillus to caspofungin results in lysis and death of hyphal apical tips and branch points where cell growth and division occur.
Pharmacodynamic effects
Caspofungin has in vitro activity against Aspergillus species (Aspergillus fumigatus [N = 75], Aspergillus flavus [N = 111], Aspergillus niger [N = 31], Aspergillus nidulans [N = 8], Aspergillus terreus [N = 52], and Aspergillus candidus [N = 3]). Caspofungin also has in vitro activity against Candida species (Candida albicans [N = 1,032], Candida dubliniensis [N = 100], Candida glabrata [N = 151], Candida guilliermondii [N = 67], Candida kefyr [N = 62], Candida krusei [N = 147], Candida lipolytica [N = 20], Candida lusitaniae [N = 80], Candida parapsilosis [N = 215], Candida rugosa [N = 1], and Candida tropicalis [N = 258]), including isolates with multiple resistance transport mutations and those with acquired or intrinsic resistance to fluconazole, amphotericin B, and 5-flucytosine. Susceptibility testing was performed according to a modification of both the Clinical and Laboratory Standards Institute (CLSI, formerly known as the National Committee for Clinical Laboratory Standards [NCCLS]) method M38-A2 (for Aspergillus species) and method M27-A3 (for Candida species).
Standardised techniques for susceptibility testing have been established for yeasts by EUCAST. EUCAST breakpoints have not yet been established for caspofungin, due to significant inter-laboratory variation in MIC ranges for caspofungin. In lieu of breakpoints, Candida isolates that ae susceptible to anidulafungin as well as micafungin should be considered susceptible to caspofungin. Similarly, C. parapsilosis isolates intermediate to anidulafungin and micafungin can be regarded intermediate to caspofungin.
Mechanism of resistance
Isolates of Candida with reduced susceptibility to caspofungin have been identified in a small number of patients during treatment (MICs for caspofungin >2 mg/L (4- to 30-fold MIC increases) have been reported using standardized MIC testing techniques approved by the CLSI). The mechanism of resistance identified is FKS1 and/or FKS2 (for C. glabrata) gene mutation. These cases have been associated with poor clinical outcomes.
Development of in vitro resistance to caspofungin by Aspergillus species has been identified. In limited clinical experience, resistance to caspofungin in patients with invasive aspergillosis has been observed. The mechanism of resistance has not been established. The incidence of resistance to caspofungin by various clinical isolates of
Candida and Aspergillus is rare.
Clinical efficacy and safety
Invasive Candidiasis in Adult Patients: Two hundred thirty-nine patients were enrolled in an initial study to compare caspofungin and amphotericin B for the treatment of invasive candidiasis. Twentyfour patients had neutropaenia. The most frequent diagnoses were bloodstream infections (candidaemia) (77 %, n=186) and Candida peritonitis (8 %, n=19); patients with Candida endocarditis, osteomyelitis, or meningitis were excluded from this study. Caspofungin 50 mg once daily was administered following a 70 mg loading dose, while amphotericin B was administered at 0.6 to 0.7 mg/kg/day to non-neutropaenic patients or 0.7 to 1.0 mg/kg/day to neutropaenic patients. The mean duration of intravenous therapy was 11.9 days, with a range of 1 to 28 days. A favourable response required both symptom resolution and microbiological clearance of the Candida infection. Two hundred twenty-four patients were included in the primary efficacy analysis (MITT analysis) of response at the end of IV study therapy; favourable response rates for the treatment of invasive candidiasis were comparable for caspofungin (73 % [80/109]) and amphotericin B (62 % [71/115]) [% difference 12.7 (95.6 % CI -0.7, 26.0)]. Among patients with candidaemia, favourable response rates at the end of IV study therapy were comparable for caspofungin (72 % [66/92]) and amphotericin B (63 % [59/94]) in the primary efficacy analysis (MITT analysis) [% difference 10.0 (95.0 % CI -4.5, 24.5)]. Data in patients with non-blood sites of infection were more limited. Favourable response rates in neutropaenic patients were 7/14 (50 %) in the caspofungin group and 4/10 (40 %) in the amphotericin B group. These limited data are supported by the outcome of the empirical therapy study.
In a second study, patients with invasive candidiasis received daily doses of caspofungin at 50 mg/day (following a 70-mg loading dose on Day 1) or caspofungin at 150 mg/day (see section 4.8). In this study, the caspofungin dose was administered over 2 hours (instead of the routine 1-hour administration). The study excluded patients with suspected Candida endocarditis, meningitis, or osteomyelitis. As this was a primary therapy study, patients who were refractory to prior antifungal agents were also excluded. The number of neutropenic patients enrolled in this study was also limited (8.0 %). Efficacy was a secondary endpoint in this study. Patients who met the entry criteria and received one or more doses of caspofungin study therapy were included in the efficacy analysis. The favorable overall response rates at the end of caspofungin therapy were similar in the 2 treatment groups: 72 % (73/102) and 78 % (74/95) for the caspofungin 50-mg and 150-mg treatment groups, respectively (difference 6.3 % [95 % CI -5.9, 18.4]).
Invasive Aspergillosis in Adult Patients: Sixty-nine adult patients (age 18-80) with invasive aspergillosis were enrolled in an open-label, non-comparative study to evaluate the safety, tolerability, and efficacy of caspofungin. Patients had to be either refractory to (disease progression or failure to improve with other antifungal therapies given for at least 7 days) (84 % of the enrolled patients) or intolerant of (16 % of enrolled patients) other standard antifungal therapies. Most patients had underlying conditions (haematologic malignancy [N = 24], allogeneic bone marrow transplant or stem cell transplant [N = 18], organ transplant [N = 8], solid tumour [N = 3], or other conditions [N = 10]). Stringent definitions, modelled after the Mycoses Study Group Criteria, were used for diagnosis of invasive aspergillosis and for response to therapy (favourable response required clinically significant improvement in radiographs as well as in signs and symptoms). The mean duration of therapy was 33.7 days, with a range of 1 to 162 days. An independent expert panel determined that 41 % (26/63) of patients receiving at least one dose of caspofungin had a favourable response. For those patients who received more than 7 days of therapy with caspofungin, 50 % (26/52) had a favourable response. The favourable response rates for patients who were either refractory to or intolerant of previous therapies were 36 % (19/53) and 70 % (7/10), respectively. Although the doses of prior antifungal therapies in 5 patients enrolled as refractory were lower than those often administered for invasive aspergillosis, the favourable response rate during therapy with caspofungin was similar in these patients to that seen in the remaining refractory patients (2/5 versus 17/48, respectively). The response rates among patients with pulmonary disease and extrapulmonary disease were 47 % (21/45) and 28 % (5/18), respectively. Among patients with extrapulmonary disease, 2 of 8 patients who also had definite, probable, or possible CNS involvement had a favourable response.
Empirical Therapy in Febrile, Neutropaenic Adult Patients: A total of 1,111 patients with persistent fever and neutropaenia were enrolled in a clinical study and treated with either caspofungin 50 mg once daily following a 70 mg loading dose or liposomal amphotericin B 3.0 mg/kg/day. Eligible patients had received chemotherapy for malignancy or had undergone hematopoietic stem-cell transplantation, and presented with neutropaenia (<500 cells/mm3 for 96 hours) and fever (>38.0°C) not responding to >96 hours of parenteral antibacterial therapy. Patients were to be treated until up to 72 hours after resolution of neutropaenia, with a maximum duration of 28 days. However, patients found to have a documented fungal infection could be treated longer. If the drug was well tolerated but the patient’s fever persisted and clinical condition deteriorated after 5 days of therapy, the dosage of study drug could be increased to 70 mg/day of caspofungin (13.3 % of patients treated) or to 5.0 mg/kg/day of liposomal amphotericin B (14.3 % of patients treated). There were 1,095 patients included in the primary Modified Intention-To-Treat (MITT) efficacy analysis of overall favourable response; caspofungin (33.9 %) was as effective as liposomal amphotericin B (33.7 %) [% difference 0.2 (95.2 % CI -5.6, 6.0)]. An overall favourable response required meeting each of 5 criteria:
(1) successful treatment of any baseline fungal infection (caspofungin 51.9 % [14/27], liposomal amphotericin B 25.9 % [7/27]), (2) no breakthrough fungal infections during administration of study drug or within 7 days after completion of treatment (caspofungin 94.8 % [527/556], liposomal amphotericin B 95.5 % [515/539]), (3) survival for 7 days after completion of study therapy (caspofungin 92.6 % [515/556], liposomal amphotericin B 89.2 % [481/539]), (4) no discontinuation from the study drug because of drug-related toxicity or lack of efficacy (caspofungin 89.7 % [499/556], liposomal amphotericin B 85.5 % [461/539]), and (5) resolution of fever during the period of neutropaenia (caspofungin 41.2 % [229/556], liposomal amphotericin B 41.4 % [223/539]).
Response rates to caspofungin and liposomal amphotericin B for baseline infections caused by Aspergillus species were, respectively, 41.7 % (5/12) and 8.3 % (1/12), and by Candida species were 66.7 % (8/12) and 41.7 % (5/12). Patients in the caspofungin group experienced breakthrough infections due to the following uncommon yeasts and moulds: Trichosporon species (1), Fusarium species (1), Mucor species (1), and Rhizopus species (1).
Paediatric population
The safety and efficacy of caspofungin was evaluated in paediatric patients 3 months to 17 years of age in two prospective, multicenter clinical trials. The study design, diagnostic criteria, and criteria for efficacy assessment were similar to the corresponding studies in adult patients (see section 5.1)..
The first study, which enrolled 82 patients between 2 to 17 years of age, was a randomized, doubleblind study comparing caspofungin (50 mg/m2 IV once daily following a 70-mg/m2 loading dose on Day 1 [not to exceed 70 mg daily]) to liposomal amphotericin B (3 mg/kg IV daily) in a 2:1 treatment fashion (56 on caspofungin, 26 on liposomal amphotericin B) as empirical therapy in paediatric patients with persistent fever and neutropenia. The overall success rates in the MITT analysis results, adjusted by risk strata, were as follows: 46.6 % (26/56) for caspofungin and 32.2 % (8/25) for liposomal amphotericin B.
The second study was a prospective, open-label, non-comparative study estimating the safety and efficacy of caspofungin in paediatric patients (ages 6 months to 17 years) with invasive candidiasis, esophageal candidiasis, and invasive aspergillosis (as salvage therapy). Forty-nine patients were enrolled and received caspofungin at 50 mg/m2 IV once daily following a 70-mg/m2 loading dose on Day 1 (not to exceed 70 mg daily), of whom 48 were included in the MITT analysis. Of these, 37 had invasive candidiasis, 10 had invasive aspergillosis, and 1 patient had esophageal candidiasis. The favorable response rate, by indication, at the end of caspofungin therapy was as follows in the MITT analysis: 81 % (30/37) in invasive candidiasis, 50 % (5/10) in invasive aspergillosis, and 100 % (1/1) in esophageal candidiasis.
5.2 Pharmacokinetic properties
Distribution
Caspofungin is extensively bound to albumin. The unbound fraction of caspofungin in plasma varies from 3.5 % in healthy volunteers to 7.6 % in patients with invasive candidiasis. Distribution plays the prominent role in caspofungin plasma pharmacokinetics and is the rate-controlling step in both the alpha- and beta-disposition phases. The distribution into tissues peaked at 1.5 to 2 days after dosing when 92 % of the dose was distributed into tissues. It is likely that only a small fraction of the caspofungin taken up into tissues later returns to plasma as parent compound. Therefore, elimination occurs in the absence of a distribution equilibrium, and a true estimate of the volume of distribution of caspofungin is currently impossible to obtain.
Biotransformation
Caspofungin undergoes spontaneous degradation to an open ring compound. Further metabolism involves peptide hydrolysis and N-acetylation. Two intermediate products, formed during the degradation of caspofungin to this open ring compound, form covalent adducts to plasma proteins resulting in a low-level, irreversible binding to plasma proteins.
In vitro studies show that caspofungin is not an inhibitor of cytochrome P450 enzymes 1A2, 2A6, 2C9, 2C19, 2D6 or 3A4. In clinical studies, caspofungin did not induce or inhibit the CYP3A4 metabolism of other medicinal products. Caspofungin is not a substrate for P-glycoprotein and is a poor substrate for cytochrome P450 enzymes.
Elimination
The elimination of caspofungin from plasma is slow with a clearance of 10-12 ml/min. Plasma concentrations of caspofungin decline in a polyphasic manner following single 1-hour intravenous infusions. A short alpha-phase occurs immediately post-infusion, followed by a beta-phase with a halflife of 9 to 11 hours. An additional gamma-phase also occurs with a half-life of 45 hours. Distribution, rather than excretion or biotransformation, is the dominant mechanism influencing plasma clearance.
Approximately 75 % of a radioactive dose was recovered during 27 days: 41 % in urine and 34 % in faeces. There is little excretion or biotransformation of caspofungin during the first 30 hours after administration. Excretion is slow and the terminal halflife of radioactivity was 12 to 15 days. A small amount of caspofungin is excreted unchanged in urine (approximately 1.4 % of dose).
Caspofungin displays moderate non-linear pharmacokinetics with increased accumulation as the dose is increased, and a dose dependency in the time to reach steady state upon multiple-dose administration.
Special populations
Increased caspofungin exposure was seen in adult patients with renal impairment and mild liver impairment, in female subjects, and in the elderly. Generally the increase was modest and not large enough to warrant dosage adjustment. In adult patients with moderate liver impairment or in higher weight patients, a dosage adjustment may be necessary (see below).
Weight:
Weight was found to influence caspofungin pharmacokinetics in the population pharmacokinetic analysis in adult candidiasis patients. The plasma concentrations decrease with increasing weight. The average exposure in an adult patient weighing 80 kg was predicted to be about 23 % lower than in an adult patient weighing 60 kg (see section 4.2).
Hepatic impairment:
In adult patients with mild and moderate hepatic impairment, the AUC is increased about 20 and 75 %, respectively. There is no clinical experience in adult patients with severe hepatic impairment and in paediatric patients with any degree of hepatic impairment. In a multiple-dose study, a dose reduction of the daily dose to 35 mg in adult patients with moderate hepatic impairment has been shown to provide an AUC similar to that obtained in adult subjects with normal hepatic function receiving the standard regimen (see section 4.2).
Renal impairment:
In a clinical study of single 70 mg doses, caspofungin pharmacokinetics were similar in adult volunteers with mild renal impairment (creatinine clearance 50 to 80 ml/min) and control subjects. Moderate (creatinine clearance 31 to 49 ml/min), advanced (creatinine clearance 5 to 30 ml/min), and end-stage (creatinine clearance <10 ml/min and dialysis dependent) renal impairment moderately increased caspofungin plasma concentrations after single-dose administration (range: 30 to 49 % for AUC). However, in adult patients with invasive candidiasis, oesophageal candidiasis, or invasive aspergillosis who received multiple daily doses of caspofungin 50 mg, there was no significant effect of mild to advanced renal impairment on caspofungin concentrations. No dosage adjustment is necessary for patients with renal impairment. Caspofungin is not dialysable, thus supplementary dosing is not required following haemodialysis.
Gender:
Caspofungin plasma concentrations were on average 17-38 % higher in women than in men.
Elderly:
A modest increase in AUC (28 %) and C24h (32 %) was observed in elderly male subjects compared with young male subjects. In patients who were treated empirically or who had invasive candidiasis, a similar modest effect of age was seen in older patients relative to younger patients.
Race:
Patient pharmacokinetic data indicated that no clinically significant differences in the pharmacokinetics of caspofungin were seen among Caucasians, Blacks, Hispanics, and Mestizos.
Paediatric Patients:
In adolescents (ages 12 to 17 years) receiving caspofungin at 50 mg/m2 daily (maximum 70 mg daily), the caspofungin plasma AUC0-24 h was generally comparable to that seen in adults receiving caspofungin at 50 mg daily. All adolescents received doses >50 mg daily, and, in fact, 6 of 8 received the maximum dose of 70 mg/day.
The caspofungin plasma concentrations in these adolescents were reduced relative to adults receiving 70 mg daily, the dose most often administered to adolescents.
In children (ages 2 to 11 years) receiving caspofungin at 50 mg/m2 daily (maximum 70 mg daily), the caspofungin plasma AUC0-24 hr after multiple doses was comparable to that seen in adults receiving caspofungin at 50 mg/day.
In young children and toddlers (ages 12 to 23 months) receiving caspofungin at 50 mg/m2 daily (maximum 70 mg daily), the caspofungin plasma AUC0-24 hr after multiple doses was comparable to that seen in adults receiving caspofungin at 50 mg daily and to that in older children (2 to 11 years of age) receiving the 50 mg/m2 daily dose.
Overall, the available pharmacokinetic, efficacy, and safety data are limited in patients 3 to 10 months of age. Pharmacokinetic data from one 10-month old child receiving the 50 mg/m2 daily dose indicated an AUC0-24 hr within the same range as that observed in older children and adults at the 50 mg/m2 and the 50 mg dose, respectively, while in one 6-month old child receiving the 50 mg/m2 dose, the AUC0-24 hr was somewhat higher.
In neonates and infants (<3 months) receiving caspofungin at 25 mg/m2 daily (corresponding mean daily dose of 2.1 mg/kg), caspofungin peak concentration (C1 hr) and caspofungin trough concentration (C24 hr) after multiple doses were comparable to that seen in adults receiving caspofungin at 50 mg daily. On Day 1, C hr was comparable and C24 hr modestly elevated (36 %) in these neonates and infants relative to adults. However, variability was seen in both C h (Day 4 geometric mean 11.73 gg/ml, range 2.63 to 22.05 gg/ml) and C24 h (Day 4 geometric mean 3.55 gg/ml, range
0.13 to 7.17 gg/ml). AUC0-24 hr measurements were not performed in this study due to the sparse plasma sampling. Of note, the efficacy and safety of caspofungin have not been adequately studied in prospective clinical trials involving neonates and infants under 3 months of age.
5.3 Preclinical safety data
Repeated dose toxicity studies in rats and monkeys using doses up to 7-8 mg/kg given intravenously showed injection site reactions in rats and monkeys, signs of histamine release in rats, and evidence of adverse effects directed at the liver in monkeys. Developmental toxicity studies in rats showed that caspofungin caused decreases in foetal body weights and an increase in the incidence of incomplete ossification of vertebra, sternebra, and skull bone at doses of 5 mg/kg that were coupled to adverse maternal effects such as signs of histamine release in pregnant rats. An increase in the incidence of cervical ribs was also noted. Caspofungin was negative in in vitro assays for potential genotoxicity as well as in the in vivo mouse bone marrow chromosomal test. No long-term studies in animals have been performed to evaluate the carcinogenic potential. For caspofungin, there were no effects on fertility in studies conducted in male and female rats up to 5 mg/kg/day.
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
Sucrose
Mannitol (E421)
Succinic acid (E363)
Sodium hydroxide (for pH adjustment) (E524)
6.2 Incompatibilities
Do not mix with diluents containing glucose, as Caspofungin is not stable in diluents containing glucose.
In the absence of compatibility studies, this medicinal product must not be mixed with other medicinal products.
6.3 Shelf life
2 years
Reconstituted concentrate: should be used immediately.
Stability data have shown that the concentrate for solution for infusion can be stored for up to 24 hours when the vial is stored at 25°C or less and reconstituted with water for injection.
Diluted patient infusion solution: should be used immediately.
Stability data have shown that the product can be used within 24 hours when stored at 25°C or less, or within 48 hours when the intravenous infusion bag (bottle) is stored refrigerated (2 to 8°C) and diluted with sodium chloride solution 9 mg/ml (0.9 %), 4.5 mg/ml (0.45 %), or 2.25 mg/ml (0.225 %) for infusion, or lactated Ringer’s solution.
From a microbiological point of view, the product should be used immediately. If not used immediately, in-use storage times and conditions prior to use are the responsibility of the user and would normally not be longer than 24 hours at 2 to 8°C, unless reconstitution/dilution has taken place in controlled and validated aseptic conditions.
6.4 Special precautions for storage
Unopened vials: store and transport refrigerated (2°C - 8°C).
For storage conditions after reconstitution and dilution of the medicinal product, see section 6.3.
6.5 Nature and contents of container
15 ml Type I glass vial with a grey bromobutyl stopper and a transparent (50 mg) / orange (70 mg) aluminium flipp-off cap.
Supplied in packs of 1 vial.
6.6 Special precautions for disposal and other handling Reconstitution of Caspofungin 70 mg
DO NOT USE ANY DILUENTS CONTAINING GLUCOSE as Caspofungin is not stable in diluents containing glucose. DO NOT MIX OR CO-INFUSE Caspofungin WITH ANY OTHER MEDICINES, as there are no data available on the compatibility of Caspofungin with other intravenous substances, additives, or
medicinal products. Visually inspect the infusion solution for particulate matter or discolouration.
Any unused medicinal product or waste material should be disposed of in accordance with local requirements.
INSTRUCTIONS FOR USE IN ADULT PATIENTS Step 1 Reconstitution of conventional vials
To reconstitute the powder bring the vial to room temperature and aseptically add 10.5 ml of water for injection. The concentrations of the reconstituted vials will be
7.2 mg/ml.
The white to off-white compact lyophilised powder will dissolve completely. Mix gently until a clear, colorless to slightly yellow solution is obtained. Reconstituted solutions should be visually inspected for particulate matter or discolouration. This reconstituted solution may be stored for up to 24 hour at or below 25°C.
Step 2 Addition of reconstituted Caspofungin to patient infusion solution
Diluents for the final solution for infusion are: sodium chloride solution for injection, or lactated Ringer’s solution. The solution for infusion is prepared by aseptically adding the appropriate amount of reconstituted concentrate (as shown in the table below) to a 250 ml infusion bag or bottle. Reduced volume infusions in 100 ml may be used, when medically necessary, for 50 mg or 35 mg daily doses.
Do not use if the solution is cloudy or has precipitated.
PREPARATION OF THE SOLUTION FOR INFUSION IN ADULTS
|
DOSE* |
Volume of reconstituted Caspofungin for transfer to intravenous bag or bottle |
Standard preparation (reconstituted Caspofungin added to 250 ml) final concentration |
Reduced volume infusion (reconstituted Caspofungin added to 100 ml) final concentration |
|
70 mg |
10 ml |
0.28 mg/ml |
Not recommended |
|
70 mg (from 2 50-mg vials)** |
14 ml |
0.28 mg/ml |
Not recommended |
|
35 mg for moderate hepatic impairment (from one 70 mg vial) |
5 ml |
0.14 mg/ml |
0.34 mg/ml |
|
* 10.5 ml shoulc |
be used for reconstitution o |
f all vials | |
** If 70 mg vial is not available, the 70 mg dose can be prepared from two 50-mg vials
INSTRUCTIONS FOR USE IN PAEDIATRIC PATIENTS
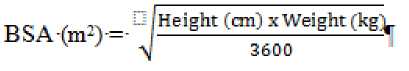
Calculation of Body Surface Area (BSA) for paediatric dosing
Before preparation of infusion, calculate the body surface area (BSA) of the patient using the following formula: (Mosteller1 Formula)

Preparation of the 70 mg/m2 infusion for paediatric patients >3 months of age (using a 70-ms vial)
1. Determine the actual loading dose to be used in the paediatric patient by using the patient's BSA (as calculated above) and the following equation:
BSA (m2) X 70 mg/m2 = Loading Dose
The maximum loading dose on Day 1 should not exceed 70 mg regardless of the patient's calculated dose.
2. Equilibrate the refrigerated vial of Caspofungin to room temperature.
3. Aseptically add 10.5 ml of water for injection.3 This reconstituted solution may be stored for up to 24 hours at or below 25°C.b This will give a final caspofungin concentration in the vial of 7.2 mg/ml.
4. Remove the volume of medicine equal to the calculated loading dose (Step 1) from the vial.
Aseptically transfer this volume (ml)c of reconstituted Caspofungin to an IV bag (or bottle) containing 250 ml of 0.9 %, 0.45 %, or 0.225 % Sodium Chloride Injection, or Lactated Ringers Injection. Alternatively, the volume (ml)c of reconstituted Caspofungin can be added to a reduced volume of 0.9 %, 0.45 %, or
0.225 % Sodium Chloride Injection or Lactated Ringers Injection, not to exceed a final concentration of 0.5 mg/ml. This infusion solution must be used within 24 hours if stored at or below 25°C or within 48 hours if stored refrigerated at 2 to 8°C.
Preparation of the 50 mg/m2 infusion for paediatric patients >3 months of age
(using a 70-mg vial)
1. Determine the actual daily maintenance dose to be used in the paediatric patient by using the patient's BSA (as calculated above) and the following equation:
BSA (m2) X 50 mg/m2 = Daily Maintenance Dose
The daily maintenance dose should not exceed 70 mg regardless of the patient's calculated dose.
2. Equilibrate the refrigerated vial of Caspofungin to room temperature.
3. Aseptically add 10.5 ml of water for injection." This reconstituted solution may be stored for up to 24 hours at or below 25°C.b This will give a final caspofungin concentration in the vial of 7.2 mg/ml.
4. Remove the volume of medicine equal to the calculated daily maintenance dose (Step 1) from the vial. Aseptically transfer this volume (ml)c of reconstituted Caspofungin to an IV bag (or bottle) containing 250 ml of 0.9 %, 0.45 %, or 0.225 % Sodium Chloride Injection, or Lactated Ringers Injection. Alternatively, the volume (ml)c of reconstituted Caspofungin can be added to a reduced volume of 0.9 %, 0.45 %, or 0.225 % Sodium Chloride Injection or Lactated Ringers Injection, not to exceed a final concentration of 0.5 mg/ml. This infusion solution must be used within 24 hours if stored at or below 25°C or within 48 hours if stored refrigerated at 2 to 8°C.
Preparation notes:
a. The white to off-white cake will dissolve completely. Mix gently until a clear, colorless to slightly yellow solution is obtained.
b. Visually inspect the reconstituted solution for particulate matter or discoloration during reconstitution and prior to infusion. Do not use if the solution is cloudy or has precipitated.
c. Caspofungin is formulated to provide the full labeled vial dose (70 mg) when 10 ml is withdrawn from the vial.
1 Mosteller RD: Simplified Calculation of Body Surface Area. N Engl J Med 1987 Oct 22;317(17): 1098 (letter)
7 MARKETING AUTHORISATION HOLDER
Regiomedica GmbH Spitalstr. 22 79539 Lorrach Germany
8 MARKETING AUTHORISATION NUMBER(S)
PL 20373/0054
9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
25/10/2016
10 DATE OF REVISION OF THE TEXT
25/10/2016