Evorel Sequi
Out of date information, search anotherPACKAGE LEAFLET: INFORMATION FOR THE USER
Evorel Sequi
Estradiol Hemihydrate, norethisterone acetate
Evorel is a registered trademark
Read all of this leaflet carefully before you start using this medicine.
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them even if their symptoms are the same as yours
• If you get any side effects and they become serious or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
In this leaflet
1. What Evorel Sequi is and what it is used for
2. Before you use Evorel Sequi
3. Safety of HRT
4. How to use Evorel Sequi
5. Possible side effects
6. How to store Evorel Sequi
7. Further information
1. What Evorel Sequi is and what it is used for
The name of your medicine is Evorel Sequi. It belongs to a group of medicines called hormone replacement therapy (HRT).
Evorel Sequi contains two medicines:
• An oestrogen (estradiol)
• A progestogen (norethisterone)
They are both female hormones.
Evorel Sequi comes in a ‘memory pack'. This can be used to help you remember when to change your patches. Each pack contains eight patches:
• Four ‘Evorel 50' patches marked CE50 (containing estradiol only)
• Four ‘Evorel Conti' patches marked CEN1 (containing estradiol and norethisterone).
The hormones are spread evenly in each patch.
They pass slowly into your body through the skin.
What Evorel Sequi is used for
Evorel Sequi is used:
• For the symptoms of the menopause (see ‘What is the menopause?' on the next page). It is only used in women who still have a womb. It is suitable for women who have had the menopause (postmenopausal) or who are around the time of the menopause (perimenopausal)
• To prevent osteoporosis (fragile bones) in women who have had the menopause and are most likely to have bone problems.
Evorel Sequi is only used if other medicines for osteoporosis have been tried first and they have not worked
What is the menopause?
Women produce oestrogen hormones from their ovaries throughout their adult life.
These hormones are important in sexual development and control of the menstrual cycle.
The menopause happens when the level of hormones produced by the ovaries goes down.
This is a gradual process. During this time, the levels of oestrogen can go up and down.
This can cause:
• Hot flushes, night sweats or mood swings
• Vaginal problems such as dryness or itching
• Uncomfortable or painful sexual intercourse
You may get the same symptoms if you have had your ovaries taken out in an operation.
How Evorel Sequi works
Evorel Sequi is known as ‘continuous sequential' HRT. This is because two hormones are used one after another:
• Estradiol is used by itself for two weeks
• Then estradiol and norethisterone are used together for the next two weeks
Evorel Sequi patches replace the oestrogen that is normally released by the ovaries.
However, taking an oestrogen hormone regularly may cause the lining of your womb to build up and get thicker.
• This means it is necessary to add a progestogen hormone to the oestrogen
• This helps shed the lining of the womb and stop any problems happening. Evorel Conti patches used during weeks 3 and 4 contain this progestogen
The shedding of the lining of the womb will probably give a ‘withdrawal bleed'. This will be like having a period each month. The withdrawal bleed will start during week 4, before you finish an Evorel Sequi pack.
Evorel Sequi is not a contraceptive.
2. Before you use Evorel Sequi
Do not use Evorel Sequi if:
• You are allergic to anything in the patches (listed in section 7 below)
• You have (or have ever had) or think you may have breast cancer
• You have (or are suspected of having) or ever had a cancer that is made worse by oestrogens (such as endometrial cancer)
• You have a thickening of the lining of the womb which has not been treated
• You have vaginal bleeding you cannot explain
• You have ever had blood clots in a vein (thrombosis) or a blood clot that has travelled to your lung (pulmonary embolism)
• You have problems with your blood which increases the likelihood of developing a blood clot (thrombosis) (such as protein C, protein S or antithrombin deficiency)
• You have ever had blocked arteries (arterial thrombo-embolic disease) that gave you angina or a heart attack or a stroke
• You have ( or have ever had) a liver disease and your liver function tests have not returned to normal
• You have a blood problem called “porphyria”
Do not use this medicine if any of the above applies to you. If you are not sure, talk to your doctor or pharmacist before using Evorel Sequi.
Stop using Evorel Sequi at once if any of the above appears for the first time and talk to your doctor immediately.
Evorel Sequi should not be used by children.
Medical check-ups
Before taking HRT, your doctor should ask about you and your family's medical history.
Your doctor may decide to examine your breasts or your tummy and may do an internal examination. They will only do this if it is necessary for you or if you have any special concerns.
Once you have started on HRT, see your doctor for regular check-ups (at least once a year).
At these check-ups, your doctor may discuss the benefits and risks of continuing to take HRT.
Make sure that you:
• Go for regular breast screening and cervical smear tests
• Regularly check your breasts for any changes such as dimpling of the skin, changes in the nipple or any lumps you can see or feel
Take special care with Evorel Sequi
Tell your doctor if you have ever had any of the following. You may need to have checks more often.
• Vaginal bleeding which you could not explain
• A problem caused by growth of the womb lining:
• Inside the womb (fibroids)
• Outside the womb (endometriosis)
• Thickening of the lining of the womb (endometrial hyperplasia)
• Increased risk of blood clots (see ‘Blood clots' in section 3 below)
• A family history of increased risk of cancers related to oestrogens (see ‘Breast cancer' in section 3 below)
• High blood pressure (hypertension).
Your doctor may tell you to stop using Evorel Sequi if your blood pressure goes up
• Diabetes
• Gallstones
• Migraine or severe headaches
• Systemic Lupus Erythematosus (SLE).
This is an allergic condition that causes joint pain, skin rashes and fever
• Epilepsy
• Asthma
• A disease affecting the eardrum and hearing (otosclerosis)
• Liver, heart or kidney problems
• High levels of triglycerides (a type of fat) in your blood as you may have a higher risk of pancreatitis (inflammation of the pancreas, which causes severe pain in the abdomen and back)
• Any breast problems
• History of sudden swelling of the face or throat, which may cause difficulty in swallowing or breathing, rapid swelling of the hands and feet and stomach cramps
You may still be able to use Evorel Sequi, but you should discuss this with your doctor first. Also tell your doctor if these illnesses return or get worse while you are using Evorel Sequi.
If you have had a premature menopause the risk of using HRT may be different. Talk to your doctor about the risks.
Other conditions:
• If you have brown patches on your face or body (chloasma) or have a history of them, you may need to keep out of the sun or away from sunbeds (these patches may not completely disappear again)
Taking other medicines
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines. This includes medicines that you buy without a prescription or herbal medicines.
In particular, tell your doctor or pharmacist if you are taking any of the following:
• Medicines for epilepsy such as phenobarbital, phenytoin or carbamazepine
• Certain medicines for infections such as rifampicin, rifabutin, nevirapine, efavirenz, ritonavir or nelfinavir
• Bosentan - for high blood pressure in the blood vessels of the lungs
• St. John's Wort - for depression
Taking these medicines with Evorel Sequi can stop it from working as well. Because of this you may get some bleeding like a period, when you are not expecting it.
• A medicine for epilepsy called lamotrigine. Using Evorel Sequi with lamotrigine could affect control of your epilepsy
Operations or tests
Tell your doctor if you are going to have surgery.
You may need to stop taking HRT about 4 to 6 weeks before the operation to reduce the risk of a blood clot. Your doctor will tell you when you can start taking HRT again.
If you visit a hospital or your family doctor for a blood or urine test, tell them that you are taking Evorel Sequi. This is because this medicine may affect the results of the tests.
Pregnancy and breast-feeding
Do not use this medicine if you are pregnant, think you may be pregnant or might become pregnant. This is because it may affect the baby.
If you become pregnant, contact your doctor straight away and remove the patch.
Do not use this medicine if you are breast-feeding.
Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breastfeeding.
Driving or using machines
There is no information about whether Evorel Sequi affects your ability to drive or use machines. See how this medicine affects you before you drive or use any tools or machines.
3. Safety of HRT
As well as benefits, HRT has some risks.
Consider the following when deciding to take or continue HRT.
Heart disease
HRT is not recommended for women who have had heart disease recently. If you have ever had heart disease, talk to your doctor to see if you should be taking HRT.
HRT will not help to prevent heart disease.
Studies of HRT (containing oestrogen and progestogen) have shown that women may be slightly more likely to get heart disease. If you get a pain in your chest that spreads to your arm and neck:
If you get a pain in your chest that spreads to your arm and neck:
• See a doctor as soon as possible
• Do not use any more HRT until your doctor says you can This pain may be a sign of heart disease.
Stroke
Research suggests that HRT slightly increases the risk of having a stroke. Other things that can increase the risk of stroke include:
• Getting older
• High blood pressure
• Smoking
• Drinking too much alcohol
• An irregular heartbeat
If you are worried about any of these things or if you have had a stroke in the past, talk to your doctor to see if you should take HRT.
How likely is a stroke?
Looking at women in their 50s, on average, over 5 years:
• In women not taking HRT - 3 in 1000 would be expected to have a stroke
• In women taking HRT - 4 in 1000 would be expected to have a stroke
Looking at women in their 60s, on average, over 5 years:
• In women not taking HRT - 11 in 1000 would be expected to have a stroke
• In women taking HRT - 15 in 1000 would be expected to have a stroke
If you get migraine-type headaches which you cannot explain:
• See a doctor as soon as possible
• Do not use any more HRT until your doctor says you can These headaches may be an early warning sign of a stroke.
Blood clots
HRT is not recommended for women who have ever had a blood clot.
HRT may increase the risk of blood clots in the veins (also called deep vein thrombosis or DVT), especially during the first year of taking it.
These blood clots are not always serious.
However, if a clot travels to the lungs, it can cause chest pain, breathlessness, collapse or even death. This is called pulmonary embolism or PE.
You are more likely to get a blood clot if:
• You are very overweight (BMI > 30 kg/m2)
• You have had a blood clot before
• Any of your close family have had blood clots
• You have had one or more miscarriages
• You have any blood clotting problem that needs treatment with a medicine such as warfarin
• You are off your feet for a long time because of major surgery, injury or illness
• You are going on a long journey and will not be moving about for some time
• You have a rare illness called SLE (Systemic Lupus Erythematosus)
• You have cancer
If any of these things apply to you, talk to your doctor to see if you should take HRT.
How likely is a blood clot?
Looking at women in their 50s, on average, over 5 years:
• In women not taking HRT - 3 in 1000 would be expected to get a blood clot
• In women taking HRT - 7 in 1000 would be expected to get a blood clot
Looking at women in their 60s, on average, over 5 years:
• In women not taking HRT - 8 in 1000 would be expected to get a blood clot
• In women taking HRT - 17 in 1000 would be expected to get a blood clot
If you get painful swelling in your leg, sudden chest pain or have difficulty breathing:
• See a doctor as soon as possible
• Do not use any more HRT until your doctor says you can These may be signs of a blood clot.
Breast cancer
Women who have breast cancer or have had breast cancer in the past should not take HRT.
Taking HRT slightly increases the risk of breast cancer. The risk is also slightly increased if you have a later menopause.
• Postmenopausal women taking oestrogen-only HRT for 5 years - the risk is about the same as for a woman of the same age who is still having periods over that time and not taking HRT
• Women taking oestrogen plus progestogen HRT - the risk is higher than for oestrogen-only HRT. However, oestrogen plus progestogen HRT is beneficial for the endometrium (see ‘Endometrial cancer')
For all kinds of HRT, the extra risk of breast cancer goes up the longer you take it. However, it returns to normal within about 5 years after stopping HRT.
Your risk of breast cancer is also higher if:
• You have a close relative (mother, sister or grandmother) who has had breast cancer
• You are very overweight
How likely is breast cancer?
Looking at women aged 50, on average, over the next 15 years:
• In women not taking HRT - 32 in 1000 will get breast cancer
• In women taking oestrogen-only HRT at age 50 and take it for 5 years, between 33 and 34 in
1000 will get breast cancer
• In women taking oestrogen-only HRT for 10 years - 37 in 1000 will get breast cancer
• In women taking oestrogen plus progestogen HRT at age 50 and take it for 5 years - 38 in 1000
will get breast cancer
• In women taking oestrogen plus progestogen HRT for 10 years - 51 in 1000 will get breast cancer
If you notice any changes in your breast, such as:
• Dimpling of the skin
• Changes in the nipple
• Any lumps you can see or feel
Make an appointment to see your doctor as soon as possible.
Endometrial cancer (cancer of the lining of the womb)
HRT is not recommended for women who have ever had cancer of the lining of the womb.
Taking oestrogen-only HRT for a long time can increase the risk of cancer of the lining of the womb (the endometrium). Taking a progestogen as well as the oestrogen helps to lower the extra risk.
If you still have your womb, your doctor will usually prescribe a progestogen as well as oestrogen. These may be prescribed separately or as a combined HRT product.
If you have had your womb removed (a hysterectomy), your doctor will discuss with you whether you can safely take oestrogen without a progestogen.
If you have had your womb removed because of endometriosis, any endometrium left in your body may be at risk of cancer.
This means your doctor may prescribe HRT that includes a progestogen as well as an oestrogen.
Your product, Evorel Sequi, contains a progestogen.
Evorel Sequi is only used in women who still have a womb (see Section 1 ‘What Evorel Sequi is used for').
How likely is endometrial cancer?
Looking at women aged 50 who still have a womb, on average, over the next 15 years:
• In women not taking HRT - 5 in 1000 will get endometrial cancer
• In women taking oestrogen-only HRT, the number will be 2 to 12 times higher, depending on the dose and how long you take it for
The addition of a progestogen to oestrogen-only HRT substantially reduces the risk of endometrial cancer.
If you get breakthrough bleeding or spotting, it is usually nothing to worry about, especially during the first few months of taking HRT.
But if the bleeding or spotting:
• Carries on for more than the first few months
• Starts after you have been on HRT for a while
• Carries on even after you've stopped taking HRT
Make an appointment to see your doctor as soon as possible. It could be a sign that your endometrium has become thicker.
Ovarian cancer
Ovarian cancer (cancer of the ovaries) is rare, but it is serious. It can be difficult to diagnose.
This is because there are often no obvious signs of the disease. Some studies have suggested that taking HRT for more than 5 years may increase the risk of ovarian cancer.
Dementia
Evorel Sequi and medicines like it will not stop memory loss (dementia). Women who start using medicines like Evorel Sequi after the age of 65 may have a small increase in the risk of dementia.
4. How to use Evorel Sequi
Always use Evorel Sequi exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure. Your doctor will aim to reduce your symptoms with the lowest possible dose for the shortest amount of time.
When to start using Evorel Sequi
You may put an Evorel 50 patch on at any time if:
• You have not used HRT before your menopause and no longer have menstrual periods
• Your menstrual cycles are not regular and you are not pregnant
• You are changing from HRT that does not give you a withdrawal bleed
Put an Evorel 50 patch on within 5 days of the start of bleeding if:
• You are not currently using HRT and still having regular periods
Put an Evorel 50 patch on at the end of a treatment cycle or one week after you finish using another HRT product if:
• You are changing from an HRT medicine that gives you a withdrawal bleed If you are using another type of HRT:
• The day you start will depend on the type of HRT you have been using Talk to your doctor if you are not sure which type of HRT you are using.
Using the patches
The patches need to be changed twice a week. You must use the patches in the right order.
Weeks 1 and 2
Use the four Evorel 50 patches one at a time.
Weeks 3 and 4
Use the four Evorel Conti patches one at a time.
As soon as you remove your fourth Evorel 50 patch, replace it with the first Evorel Conti patch.
Start a new pack of Evorel Sequi as soon as you finish one. Do not leave a break between packs.
Changing your patches
• You must change the patches twice a week to give your body a steady supply of hormones.
There is enough hormone in each patch to last for several days
• Change your patch on the same two days every week. This will mean that one patch is on for three days and the next patch for four days
• For example, if you apply your first patch on a Monday, change it on Thursday and again on the following Monday. You can work out your two days from the following table, starting from the first day of use:
If you put your first patch on: Change on: Change again on:
|
Monday - |
Thursday |
& |
Monday |
|
Tuesday - |
► Friday |
& |
Tuesday |
|
Wednesday |
Saturday |
& |
Wednesday |
|
Thursday |
► Sunday |
& |
Thursday |
|
Friday |
Monday |
& |
Friday |
|
& |
Saturday | ||
|
Sunday |
Wednesday |
& |
Sunday |
To help you remember your two “patch change" days, mark them here or on the pack. They are written on the pack like this:

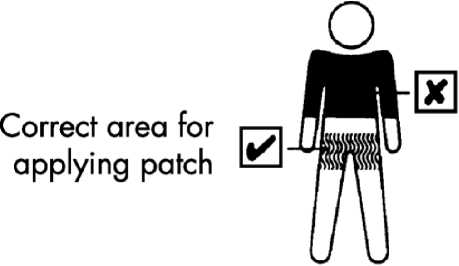
Where to apply the patch
Stick the patch onto a hairless area of skin below the waist. Most women prefer to wear the patch on the thigh or bottom.
• Do not apply on or near the breasts
• Do not put it on top of cuts, spots or anywhere the skin is irritated
• Do not use cream, moisturiser or talc before applying the patch
• Do not apply the patch on the same area of skin twice in a row
• It can be worn under loose areas of clothing
Where to apply the patch
Stick the patch onto a hairless area of skin below the waist. Most women prefer to wear the patch on the thigh or bottom.
• Do not apply on or near the breasts
• Do not put it on top of cuts, spots or anywhere the skin is irritated
• Do not use cream, moisturizer or talc before applying the patch
• Do not apply the patch on the same area of skin twice in a row
• It can be worn under loose areas of clothing
• Do not wear a patch under elasticated areas or a tight waistband
• Apply the patch to clean, dry, cool skin as soon as you open the protective pouch
If you forget to change the patch
Change it as soon as you remember and then keep to your original “patch change” days. You may get some bleeding and spotting like a period during this time.
If you use more Evorel Sequi than you should
It is unlikely that you will have too much of the hormones in Evorel Sequi. The most common symptoms of having too much oestrogen or progestogen in your body are:
• Tender breasts
• Feeling sick (nausea) or being sick
• Unexpected vaginal bleeding
• Stomach pain or bloating
Removing the patch can reverse the effects of too much oestrogen and/or progestogen. Talk to your doctor or pharmacist before using any more patches.
Contraception while using Evorel Sequi
The levels of hormone from the patches are too low to act as a contraceptive. Use non-hormonal contraceptive methods (such as a condom, diaphragm or coil) until your periods have completely stopped.
Everyday activities
• You can have a bath or shower as normal. Do not scrub too hard as this can loosen the edges of the patch
• You can go swimming. The patch will not be affected
• You can exercise and play sports. However, do not wear the patch under tight clothing or waist bands
• You can sunbathe. However, keep the patch covered, out of direct sunlight
If you have any further questions on the use of this product, ask your doctor or pharmacist.
5. Possible side effects
Like all medicines, Evorel Sequi can cause side effects, although not everybody gets them.
Take off the patch and tell your doctor straight away if you notice or suspect any of the following. You may need urgent medical treatment.
• Blood clots (thrombosis), or stroke (frequency not known)
• Yellowing of the skin or whites of the eyes (jaundice) or other liver problems
• Migraine-type headaches for the first time or more frequent (affects less than 1 in 10 people)
• An increase in blood pressure (affects less than 1 in 10 people)
• Breast or ovarian cancer, endometrial cancer or hyperplasia (long, heavy or irregular vaginal bleeding)Widespread rash with peeling skin and blistering in the mouth, eyes and genitals (Stevens-Johnson syndrome) (frequency not known)
• Convulsions or fits (frequency not known)
Tell your doctor if you notice any of the following side effects while using Evorel Sequi:
Very common (affects more than 1 in 10 people)
• Irritated, itchy, red skin where the patch is applied
Common (affects less than 1 in 10 people)
• Feeling depressed or nervous
• Inappropriate signs of emotion
• Being unable to sleep
• Headache
• Itchy skin or red rash
• Feeling sick (nausea), or having stomach pain wind or other stomach upsets
• Diarrhoea
• Pain including pain in the back, muscles, joints
• Breast pain
• Feeling generally unwell
• Weight gain
• Heavy vaginal bleeding, painful periods
• Water retention or build-up of fluid under the skin (oedema)
Uncommon (affects less than 1 in 100 people)
• Concentration problems
• Feeling dizzy
• More or less interest in sex than usual
• Allergic reaction (hypersensitivity)
• A fungal infection called thrush
• Feeling tired
• Being aware of your heartbeat (palpitations)
• Numb or tingling hands or feet, less skin sensitivity
• Breast lumps (non-cancerous)
• Fuller breasts
• Irregular vaginal bleeding
• Thickening of the lining of the womb
Frequency not known
• Mood swings
• Bloated feeling
• Gallstones
• Swelling of the hands and feet (peripheral oedema)
• Puffy skin where the patch is applied
If any of the side effects gets serious, or if you notice any other side effects not listed in this leaflet, please tell your doctor or pharmacist.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard. By reporting side effects, you can help provide more information on the safety of this medicine.
6. How to store Evorel Sequi
KEEP OUT OF THE SIGHT AND REACH OF CHILDREN. THIS ALSO APPLIES TO USED AND DISPOSED PATCHES.
Do not store above 25°C.
Do not use Evorel Sequi after the expiry date which is stated on the label. The expiry date refers to the last day of that month.
Do not use a patch if its protective pouch is open.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines that are no longer required. These measures will help to protect the environment. If your medicine becomes discoloured or shows any signs of deterioration, you should seek the advice of your pharmacist who will tell you what to do.
7. Further information
Evorel Sequi comes in a memory pack containing four Evorel 50 patches (marked CE50) and four Evorel Conti patches (marked CEN1). Both types of patch are square with rounded corners. They are clear with a sticky backing that can be stuck to the skin. Each patch comes in a protective sealed pouch and has a surface area of 16 sq cm.
The active substances in Evorel Sequi are estradiol hemihydrate and norethisterone acetate.
Each Evorel 50 patch contains 3.2 mg of estradiol hemihydrate. Each Evorel 50 patch delivers 50 micrograms of estradiol a day.
Each Evorel Conti patch contains 3.2 mg of estradiol hemihydrate and 11.2 mg of norethisterone acetate. Each Evorel Conti patch delivers 50 micrograms of estradiol and 170 micrograms of norethisterone a day.
The additional excipients are Acrylate-vinylacetate copolymer, guar gum, polyethylene terephthalate foil, siliconised polyethylene terephthalate foil.
Manufacturer
Manufactured by Janssen Pharmaceutica NV, Turnhoutseweg 30, B-2340 Beerse, Belgium. Procured from within the Eu and repackaged by the product licence holder: GPharma Ltd., Salford M50 2PU.
Putting a patch on
Do not use a patch if its protective pouch is already open.
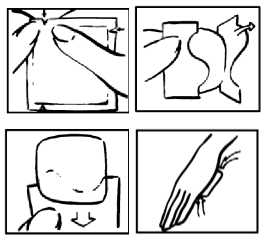
Step 1: Open and Peel
• Using the notches as a guide, tear along two edges of the pouch. Remove the patch
• With the protective backing facing you, bend and peel off half the backing. Don't touch the sticky side - it may not stick properly if you do
Step 2: Apply and Press
• Apply the open half of the patch to your skin
• Remove the remaining backing and press down the rest of the patch
• Press the patch with the palm of your hand to make sure it is firmly stuck
PL 16369/1519
Leaflet Revision: 08/10/2014
Removing a patch
• Peel an edge of the patch smoothly away from the skin
• Fold the patch in half, so that the sticky side sticks to itself
• Put it in with the household rubbish, safely out of the reach of children and pets
• Do not flush used patches down the toilet
When you remove the patch some glue may remain on your skin. It will disappear with time or you can use baby oil to remove it.

If a patch falls off
• Apply a new patch of the same type. If you have just had a bath or shower, wait until your skin cools before applying the new patch.
• It is always useful to keep a spare pack that you can use to replace patches that have fallen off. Talk to your doctor if you need more patches.