Iopidine 5mg/Ml Eye Drops
Out of date information, search anotherS1329 LEAFLET lopidine 20121026
PACKAGE LEAFLET: INFORMATION FOR THE USER IOPIDINE 5mg/ml EYE DROPS, SOLUTION (apraclonidine hydrochloride)
Your medicine is known as lopidine 5mg/ml Eye Drops, Solution but will be referred to as Iopidine throughout the following patient information leaflet.
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or your pharmacist.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
In this leaflet:
1. What Iopidine is and what it is used for
2. Before you use Iopidine
3. How to use Iopidine
4. Possible side effects
5. How to store Iopidine
6. Further information
1. WHAT IOPIDINE IS AND WHAT IT IS USED FOR
Iopidine belongs to a group of medicines known as alpha agonists. It is used in the treatment of chronic glaucoma in people who are already receiving other medicines to treat this disease.
In these people, Iopidine helps to reduce the fluid pressure in the eye and can delay the need for pressure relieving eye surgery.
2. BEFORE YOU USE IOPIDINE
Do not use Iopidine...
• If you have a history of severe or unstable heart disease or circulatory problems.
• If you are allergic to apraclonidine, clonidine or any of the ingredients listed in section 6.
• If you are currently taking monoamine oxidase inhibitors antidepressants or tricycylic antidepressants.
• If you are currently taking medicines of the class of sympathomimetics that are taken either orally or via injection.
• In CHILDREN under 12 years of age.
Ask your doctor for advice.
Take special care...
• Only use Iopidine for dropping in your eye(s).
• Iopidine may not continue to control your eye pressure after you have used them for a period of time. Your doctor will examine you often while you are using Iopidine to see whether the eye drops are still working for you.
• As Iopidine decreases the pressure in your eye(s), you should have your eye pressure checked regularly to ensure that the pressure in your eye(s) remains under control.
If you have a history of, or are taking medicine to treat, any of
the following:
• Any heart disease (including angina, heart attacks or heart failure)
• High blood pressure or other circulatory problems (including stroke, Raynaud's disease and fainting spells)
• Kidney or liver problems
• Depression
• Parkinson’s disease
• Diabetes or low blood sugar. Iopidine may hide the signs and symptoms of a sudden reduction in blood sugar such as a fast heart beat or trembling.
• If you are due to have an operation.
If any of these apply, you may still be able to use Iopidine, but
discuss it with your doctor first.
Using Iopidine with food and drink
No alcohol should be consumed during treatment with Iopidine as it can increase its effects.
Using other medicines
Tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription. Iopidine must not be used if you are taking monoamine oxidase inhibitor antidepressants or tricyclic antidepressants. Iopidine must also not be used if you are taking medicines of the class of sympathomimetics that are taken either orally or via injection. Iopidine may increase the effects of some medicines used to treat - depression - asthma - high blood pressure - heart medicines containing digoxin or digitoxin - some forms of mental illness and Parkinson's disease; and may interact with - some pain killers - sedatives - anaesthetic - tricyclic antidepressants - phenothiazines - cough and cold remedies -glaucoma medications such as timolol, brimonidine or dipivefrine -eye drops used to whiten the eye.
Pregnancy and breast-feeding
If you are pregnant or might get pregnant, or if you are breastfeeding a baby, talk to your doctor before you use Iopidine. Iopidine should not be used during pregnancy or breast-feeding. Driving and using machines
This type of medicine may cause you to feel sleepy and dizzy. If you do, you should not drive or operate machinery.
Important information if you wear Contact Lenses
Do not use the drops while wearing contact lenses. You should remove contact lenses (hard or soft) before using Iopidine and wait at least 15 minutes after use before putting your lenses back in. There is a preservative in Iopidine (benzalkonium chloride) that may cause eye irritation and is known to discolour soft contact lenses.
3. HOW TO USE IOPIDINE
The usual dose
The usual dose is 1 drop into your eye(s), 3 times each day.
Remove the loose collar from the cap when the bottle is first opened.
Always use Iopidine exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure.
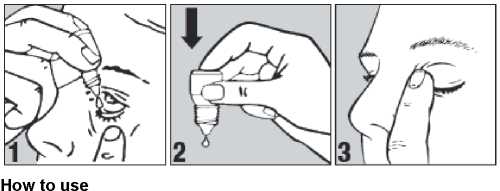
• Wash your hands before you start.
• Twist off the bottle cap.
• Hold the bottle pointing down, between your thumb and fingers.
• Tilt your head back.
• Pull down your lower eyelid with a finger until there is a 'pocket' between the eyelid and your eye. The drop will go in here (picture 1).
• Bring the bottle tip close to the eye. Do this in front of a mirror if it helps.
• Do not touch your eye or eyelid, surrounding areas or other surfaces with the dropper. It could infect the drops.
• Gently press on the base of the bottle to release one drop at a time (picture 2).
• Do not squeeze the bottle, only a gentle press on the bottom is needed.
• After using Iopidine, press a finger into the corner of your eye, by the nose (picture 3). This helps to stop Iopidine getting into the rest of the body.
• If you use drops in both eyes, repeat the steps for your other eye. Put the bottle cap firmly back on immediately after use.
• If a drop misses your eye, try again.
• If you forget to use Iopidine, continue with the next dose as planned. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule.
• Do not use a double dose to make up.
• If Iopidine is swallowed, see your doctor immediately.
* If you use more lopidine than you should rinse it all out with warm water. Do not put in any more drops until it is time for your next regular dose. In case of accidental ingestion, symptoms of overdose may include decreased blood pressure, drowsiness, decreased heart rate, hypoventilation (reduced rate and depth of breathing), and convulsion.
* If you are using other eye drop or eye ointment medicines,
leave at least 5 minutes between each medicine. Eye ointments should be administered last.
* If you have any further questions on the use of Iopidine, ask your doctor or pharmacist.
6. FURTHER INFORMATION
What Iopidine contains
• Iopidine contains 5mg/ml of the active ingredient apraclonidine (as hydrochloride).
• Iopidine also contains the following inactive ingredients: benzalkonium chloride, sodium acetate, sodium chloride and purified water.
Very small amounts of hydrochloric acid and/or sodium hydroxide may have been added to regulate the acidity/alkalinity of the product to ensure comfort in the eye.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Iopidine can cause side effects, although not everybody gets them.
Iopidine can cause allergic reactions. If you experience one or more of the following eye symptoms - redness - itching -discomfort - watery eyes - abnormal sensation - eye and eyelid swelling - poor vision - see your doctor immediately.
If your vision gets worse straight after using Iopidine, stop use and see your doctor immediately.
• You may experience some or all of the following effects in your eye(s):
Very Common (affect more than 1 person in 10): increased redness
- itching - inflammation.
Common (affect 1 to 10 people in 100): discomfort - watery eyes -swelling of the eyelids - gritty feeling in the eye - dry eye - eyelid crusting.
Uncommon (affect 1 to 10 people in 1000): bumps under the eyelids - swelling of the eye - abnormal vision - pain - inflammation and irritation of the eye or eyelids - corneal (the front part of your eye) surface damage - sensitivity to light - redness of the eyelid -raising or pulling up of the eyelids - increase in pupil size - reduced vision - blurred vision - drooping of eyelid - discharge or whitening of the eye.
• You may also experience effects in other areas of your body including:
Common: dry mouth - inflammation inside the nose - dermatitis -dry nose - weakness - headache - unusual taste.
Uncommon: chest pain - swelling of your hands, feet or extremities
- irregular heart beat - constipation - nausea - feeling tired - sore throat - runny nose - muscle aches - poor coordination - sleepiness
- dizziness - tingling feeling - nervousness - depression - difficulty sleeping - shortness of breath or difficulty breathing - unusual sense of smell - facial swelling - irritability - widening of blood vessels.
If any of the side effects get serious, or you notice any side effects not listed in this leaflet, tell your doctor or pharmacist.
What Iopidine looks like and contents of the pack
It is a clear, colourless solution in a white plastic bottle with a white
tamper evident screw cap.
Iopidine is available in 5ml plastic dropper bottles.
Product Licence holder
Procured from within the EU and repackaged by the Product Licence holder: S&M Medical Ltd, Chemilines House,
Alperton Lane, Wembley, HA0 1DX.
Manufacturer
This product is manufactured by SA Alcon-Couvreur NV, Rijksweg 14, B-2870 Puurs, Belgium.
| POM | PL No: 19488/1329 Leaflet revision date: 26 October 2012
Iopidine is a registered trade mark of Alcon Inc, Switzerland.
S1329 LEAFLET Iopidine 20121026
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Iopidine should not be stored above 25°C. Do not refrigerate or freeze. Store in the original carton to protect from light. Discard one month after first opening.
• Do not use after the expiry date printed on the carton or bottle label.
• If your doctor tells you to stop using the medicine, please take it back to the pharmacist for safe disposal. Only keep the medicine if your doctor tells you to.
• If the medicine becomes discoloured or shows any other signs of deterioration, you should seek the advice of your pharmacist who will tell you what to do.
Read all of this leaflet carefully before you start using this
medicine
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or your pharmacist.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
S1329 LEAFLET Apraclonidine 20121026
PACKAGE LEAFLET: INFORMATION FOR THE USER APRACLONIDINE 5mg/ml EYE DROPS, SOLUTION (apraclonidine hydrochloride)
Your medicine is known as Apraclonidine 5mg/ml Eye Drops, Solution but will be referred to as Apraclonidine throughout the following patient information leaflet.
In this leaflet:
1. What Apraclonidine is and what it is used for
2. Before you use Apraclonidine
3. How to use Apraclonidine
4. Possible side effects
5. How to store Apraclonidine
6. Further information
1. WHAT APRACLONIDINE IS AND WHAT IT IS USED FOR
Apraclonidine belongs to a group of medicines known as alpha agonists.
It is used in the treatment of chronic glaucoma in people who are already receiving other medicines to treat this disease.
In these people, Apraclonidine helps to reduce the fluid pressure in the eye and can delay the need for pressure relieving eye surgery.
2. BEFORE YOU USE APRACLONIDINE
Do not use Apraclonidine...
• If you have a history of severe or unstable heart disease or circulatory problems.
• If you are allergic to apraclonidine, clonidine or any of the ingredients listed in section 6.
• If you are currently taking monoamine oxidase inhibitors antidepressants or tricycylic antidepressants.
• If you are currently taking medicines of the class of sympathomimetics that are taken either orally or via injection.
• In CHILDREN under 12 years of age.
Ask your doctor for advice.
Take special care...
• Only use Apraclonidine for dropping in your eye(s).
• Apraclonidine may not continue to control your eye pressure after you have used them for a period of time. Your doctor will examine you often while you are using Apraclonidine to see whether the eye drops are still working for you.
• As Apraclonidine decreases the pressure in your eye(s), you should have your eye pressure checked regularly to ensure that the pressure in your eye(s) remains under control.
If you have a history of, or are taking medicine to treat, any of
the following:
• Any heart disease (including angina, heart attacks or heart failure)
• High blood pressure or other circulatory problems (including stroke, Raynaud's disease and fainting spells)
• Kidney or liver problems
• Depression
• Parkinson’s disease
• Diabetes or low blood sugar. Apraclonidine may hide the signs and symptoms of a sudden reduction in blood sugar such as a fast heart beat or trembling.
• If you are due to have an operation.
If any of these apply, you may still be able to use Apraclonidine, but discuss it with your doctor first.
Using Apraclonidine with food and drink
No alcohol should be consumed during treatment with Apraclonidine as it can increase its effects.
Using other medicines
Tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription. Apraclonidine must not be used if you are taking monoamine oxidase inhibitor antidepressants or tricyclic antidepressants. Apraclonidine must also not be used if you are taking medicines of the class of sympathomimetics that are taken either orally or via injection. Apraclonidine may increase the effects of some medicines used to treat - depression - asthma -high blood pressure - heart medicines containing digoxin or digitoxin - some forms of mental illness and Parkinson's disease; and may interact with - some pain killers - sedatives - anaesthetic - tricyclic antidepressants - phenothiazines - cough and cold remedies - glaucoma medications such as timolol, brimonidine or dipivefrine - eye drops used to whiten the eye.
Pregnancy and breast-feeding
If you are pregnant or might get pregnant, or if you are breastfeeding a baby, talk to your doctor before you use Apraclonidine. Apraclonidine should not be used during pregnancy or breastfeeding.
Driving and using machines
This type of medicine may cause you to feel sleepy and dizzy. If you do, you should not drive or operate machinery.
Important information if you wear Contact Lenses
Do not use the drops while wearing contact lenses. You should remove contact lenses (hard or soft) before using Apraclonidine and wait at least 15 minutes after use before putting your lenses back in. There is a preservative in Apraclonidine (benzalkonium chloride) that may cause eye irritation and is known to discolour soft contact lenses.
3. HOW TO USE APRACLONIDINE
The usual dose
The usual dose is 1 drop into your eye(s), 3 times each day. Remove the loose collar from the cap when the bottle is first opened.
Always use Apraclonidine exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure.
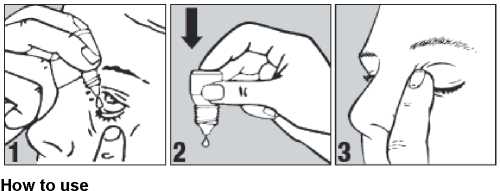
• Wash your hands before you start.
• Twist off the bottle cap.
• Hold the bottle pointing down, between your thumb and fingers.
• Tilt your head back.
• Pull down your lower eyelid with a finger until there is a 'pocket' between the eyelid and your eye. The drop will go in here (picture 1).
• Bring the bottle tip close to the eye. Do this in front of a mirror if it helps.
• Do not touch your eye or eyelid, surrounding areas or other surfaces with the dropper. It could infect the drops.
• Gently press on the base of the bottle to release one drop at a time (picture 2).
• Do not squeeze the bottle, only a gentle press on the bottom is needed.
• After using Apraclonidine, press a finger into the corner of your eye, by the nose (picture 3). This helps to stop Apraclonidine getting into the rest of the body.
• If you use drops in both eyes, repeat the steps for your other eye. Put the bottle cap firmly back on immediately after use.
• If a drop misses your eye, try again.
• If you forget to use Apraclonidine, continue with the next dose as planned. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule.
• Do not use a double dose to make up.
• If Apraclonidine is swallowed, see your doctor immediately.
• If you use more Apraclonidine than you should rinse it all out with warm water. Do not put in any more drops until it is time for your next regular dose. In case of accidental ingestion, symptoms of overdose may include decreased blood pressure, drowsiness, decreased heart rate, hypoventilation (reduced rate and depth of breathing), and convulsion.
• If you are using other eye drop or eye ointment medicines,
leave at least 5 minutes between each medicine. Eye ointments should be administered last.
• If you have any further questions on the use of
Apraclonidine, ask your doctor or pharmacist.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Apraclonidine can cause side effects, although not everybody gets them.
Apraclonidine can cause allergic reactions. If you experience one or more of the following eye symptoms - redness - itching -discomfort - watery eyes - abnormal sensation - eye and eyelid swelling - poor vision - see your doctor immediately.
If your vision gets worse straight after using Apraclonidine, stop use and see your doctor immediately.
• You may experience some or all of the following effects in your eye(s):
Very Common (affect more than 1 person in 10): increased redness
- itching - inflammation.
Common (affect 1 to 10 people in 100): discomfort - watery eyes -swelling of the eyelids - gritty feeling in the eye - dry eye - eyelid crusting.
Uncommon (affect 1 to 10 people in 1000): bumps under the eyelids - swelling of the eye - abnormal vision - pain - inflammation and irritation of the eye or eyelids - corneal (the front part of your eye) surface damage - sensitivity to light - redness of the eyelid -raising or pulling up of the eyelids - increase in pupil size - reduced vision - blurred vision - drooping of eyelid - discharge or whitening of the eye.
• You may also experience effects in other areas of your body including:
Common: dry mouth - inflammation inside the nose - dermatitis -dry nose - weakness - headache - unusual taste.
Uncommon: chest pain - swelling of your hands, feet or extremities
- irregular heart beat - constipation - nausea - feeling tired - sore throat - runny nose - muscle aches - poor coordination - sleepiness
- dizziness - tingling feeling - nervousness - depression - difficulty sleeping - shortness of breath or difficulty breathing - unusual sense of smell - facial swelling - irritability - widening of blood vessels.
If any of the side effects get serious, or you notice any side effects not listed in this leaflet, tell your doctor or pharmacist.
6. FURTHER INFORMATION
What Apraclonidine contains
• Apraclonidine contains 5mg/ml of the active ingredient apraclonidine (as hydrochloride).
• Apraclonidine also contains the following inactive ingredients: benzalkonium chloride, sodium acetate, sodium chloride and purified water.
Very small amounts of hydrochloric acid and/or sodium hydroxide may have been added to regulate the acidity/alkalinity of the product to ensure comfort in the eye.
What Apraclonidine looks like and contents of the pack
It is a clear, colourless solution in a white plastic bottle with a white tamper evident screw cap.
Apraclonidine is available in 5ml plastic dropper bottles.
Product Licence holder
Procured from within the EU and repackaged by the Product Licence holder: S&M Medical Ltd, Chemilines House,
Alperton Lane, Wembley, HA0 1DX.
Manufacturer
This product is manufactured by SA Alcon-Couvreur NV, Rijksweg 14, B-2870 Puurs, Belgium.
| POM | PL No: 19488/1329 Leaflet revision date: 26 October 2012
S1329 LEAFLET Apraclonidine 20121026
5. HOW TO STORE APRACLONIDINE
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Apraclonidine should not be stored above 25°C. Do not refrigerate or freeze. Store in the original carton to protect from light. Discard one month after first opening.
• Do not use after the expiry date printed on the carton or bottle label.
• If your doctor tells you to stop using the medicine, please take it back to the pharmacist for safe disposal. Only keep the medicine if your doctor tells you to.
• If the medicine becomes discoloured or shows any other signs of deterioration, you should seek the advice of your pharmacist who will tell you what to do.