Levobupivacaine 5 Mg/Ml Solution For Injection/Infusion

FRESENIUS
KABI

01-59-12-xxx
Package leaflet: Information for the user
Levobupivacaine 2.5 mg/ml and 5.0 mg/ml
solution for injection/infusion
Levobupivacaine
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or nurse.
• If you get any side effects, talk to your doctor or nurse.
This includes any possible side effects not listed in this leaflet.
See section 4.
The name of your medicine is Levobupivacaine 2.5 mg/ml and 5.0 mg/ml solution for injection/infusion; in the rest of the leaflet it will be called “Levobupivacaine ”
What is in this leaflet:
1. What Levobupivacaine is and what it is used for
2. What you need to know before you are given Levobupivacaine
3. How you will be given Levobupivacaine
4. Possible side effects
5. How to store Levobupivacaine
6. Contents of the pack and other information
1. What Levobupivacaine is and what it is used for
Levobupivacaine belongs to a group of medicines called local anaesthetics. This type of medicine is used to make an area of the body numb or free from pain.
In adults:
Levobupivacaine is used as a local anaesthetic to numb parts of the body before major surgery (for example as an epidural for caesarean section) and minor surgery.
It is also used for pain relief
• after major surgery
• during childbirth
2. What you need to know before you are given Levobupivacaine
Do not use Levobupivacaine :
• if you are allergic (hypersensitive) to levobupivacaine, to any similar local anaesthetics or to any of the other ingredients of this medicine (listed in section 6).
• if you have very low blood pressure
• to numb an area by injecting Levobupivacaine into a vein
• As a type of pain relief given by injection into the area around the neck of the womb (the cervix) during the early stage of labour (paracervical block)
Warnings and precautions
Talk to your doctor before you are given Levobupivacaine if you have any of the diseases or conditions below. You may need to be checked more closely or given a smaller dose.
• if you have a heart condition
• if you suffer from diseases of the nervous system
• if you are weak or ill
• if you are elderly
• if you have liver disease.
Other medicines and Levobupivacaine
Tell your doctor or nurse if you are taking, have recently taken or might take any other medicines. In particular, tell them if you are taking medicines for:
• irregular heart beats (such as mexiletine)
• fungal infections (such as ketoconazole) since this may affect how long Levobupivacaine stays in your body
• asthma (such as theophylline) since this may affect how long Levobupivacaine stays in your body.
Pregnancy and breastfeeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
Levobupivacaine must not be given for pain relief by injection into the area around the neck of the womb or cervix during childbirth (paracervical block).
The effect of Levobupivacaine on the child during the early stages of pregnancy is not known. Therefore, Levobupivacaine should not be used during the first three months of your pregnancy, unless your doctor thinks it is necessary.
It is not known if levobupivacaine passes into breast milk. However from the experience with a similar drug, only small amounts of levobupivacaine are expected to pass into breast milk. Breastfeeding is therefore possible after having a local anaesthetic.
Driving and using machines
The use of Levobupivacaine can have a considerable effect on the ability to drive or use machines. You must not drive or operate machinery until all the effects of Levobupivacaine and the immediate effects of surgery have worn off. Make sure you get advice about this matter from the doctor or nurse who is treating you, before leaving hospital.
Levobupivacaine contains sodium
This medicinal product contains 1.57 mmol (or 36 mg) sodium per ampoule of 10 ml solution. To be taken into consideration by patients on a controlled sodium diet.
3. How to use Levopubivacaine
Your doctor will give you Levobupivacaine by injection through a needle or into a small tube in your back (epidural). Levobupivacaine can also be injected into other parts of the body to numb the area that you will have treated, such as arm or leg.
Your doctor and nurse will watch you carefully while you are being given Levobupivacaine .
Dosage
The amount of Levobupivacaine you will be given and how often it is given will depend on why it is being used and also on your health, age and weight. The smallest dose that can produce numbness in the required area will be used. The dose will be carefully worked out by your doctor.
When Levobupivacaine is used for pain relief during labour or for childbirth by caesarean section (an epidural), the dose used should be particularly carefully controlled.
If you get more Levobupivacaine than you should
If you get more Levobupivacaine than you should, you may have numbness of the tongue, dizziness, blurred vision, muscle twitching, severe breathing difficulties (including stopping breathing) and even fits (convulsions). If you notice any of these symptoms, tell your doctor immediately. Sometimes too much Levobupivacaine may also cause low blood pressure, fast or slow heartbeats and changes in your heart rhythm. Your doctor may need to give you other medicines to help stop these symptoms.
If you have any further questions on the use of this medicine, ask your doctor or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Tell your doctor or nurse immediately if you notice any of the following side effects. Some side effects with Levobupivacaine can be serious.
V001
only. Discard any unused solution.
Method of administration
Levobupivacaine should be administered only by, or under the supervision of, a clinician having the necessary training and experience.
Please refer to the summary of product characteristics for posology information.
Careful aspiration before and during injection is recommended to prevent intravascular injection.
Aspiration should be repeated before and during administration of a bolus dose, which should be injected slowly and in incremental doses, at a rate of 7.5-30 mg/min, while closely observing the patient's vital functions and maintaining verbal contact.
If toxic symptoms occur, the injection should be stopped immediately.
V001
Do not use unless the container is undamaged.
The solution/dilution should be inspected visually prior to use. Only clear solutions without visible particles should be used.
A sterile blister container should be chosen when a sterile ampoule surface is required. Ampoule surface is not sterile if sterile blister is pierced.
Dilutions of levobupivacaine standard solutions should be made with sodium chloride 9 mg/ml (0.9%) solution for injection using aseptic techniques.
Clonidine 8.4 mg/ml, morphine 0.05 mg/ml and fentanyl 4 mg/ml have been shown to be compatible with levobupivacaine in sodium chloride 9 mg/ml (0.9%) solution for injection. Shelf life after first opening: The product should be used immediately.
Shelf life after dilution:
Chemical and physical in-use stability has been demonstrated for Levobupivacaine diluted with sodium chloride 9 mg/ml (0.9%) solution to a final concentration of 0.625 mg/ml and 1.25 mg/ml, respectively for 30 days either 2-8°C or 20°C - 25°C.
Chemical and physical in-use stability has been demonstrated for Levobupivacaine diluted with sodium chloride 9 mg/ml (0.9%) to a final concentration of 0.625 mg/ml and 1.25 mg/ml, respectively
- With 8.4 pg/ml clonidine hydrochloride, 50 pg/ml morphine sulfate and 2-4 pg/ml fentanyl citrate for 30 days at either 2-8°C or 20°C-25°C .
- With sufentanil added in the concentration of 0.4 pg/ml for 30 days at 2-8 °C or 7 days at 20 °C-25 °C.
From a microbiological point of view, the product should be used immediately. If not used immediately, in-use storage times and conditions prior to use are the responsibility of the user and would normally not be longer than 24 hours at 2 to 8c, unless the dilution and admix have taken place in controlled and validated aseptic conditions.
Levobupivacaine must not be mixed with any other medicinal products except those listed above. Dilution with alkaline solutions such as sodium bicarbonate may result in precipitation.
Very common (may affect more than 1 in 10 people):
• feeling tired or weak, short of breath, looking pale (these are all signs of anaemia)
• low blood pressure
• nausea
Common (may affect up to 1 in 10 people):
• dizziness
• headache
• vomiting
• problems (distress) for an unborn child
• back pain
• high body temperature (fever)
• pain after surgery
Not known (frequency cannot be estimated from the available data):
• serious allergic (hypersensitive) reactions which cause severe breathing difficulties, difficulty in swallowing, hives and very low blood pressure.
• allergic (hypersensitive) reactions recognised by red itchy skin, sneezing, sweating a lot, rapid heartbeat, fainting or swelling of the face, lips, mouth, tongue or throat.
• loss of consciousness
• drowsiness
• blurred vision
• breathing stopping
• heart block or heart stopping
• localised tingling
• numbness of the tongue
• muscle weakness or twitching
• loss of bladder or bowel control
• paralysis
• fits (convulsions)
• tingling, numbness or other abnormal sensation
• prolonged erection of the penis that may be painful
• nerve disorder which can include drooping of the eyelid, small pupil (black center of the eye), sunken eye socket, sweating and/or redness in one side of the face
Fast, slow or irregular heartbeats, and heart rhythm changes that can be seen on an ECG, have also been reported as side effects.
Rarely, some side effects may be long-term or permanent.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly:
For UK: via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard For IE: Reports may be made by following the links to the online reporting option accessible from the IMB homepage, or by completing the downloadable report form also accessible from the IMB website, which may be completed manually and submitted to the IMB via freepost, to the following address:
FREEPOST
IMB Pharmacovigilance
Earlsfort Terrace
IRL - Dublin 2
Tel: +353 1 6764971
Fax: +353 1 6762517
Website: www.imb.ie
e-mail: imbpharmacovigilance@imb.ie
By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Levobupivacaine
Keep this medicine out of the sight and reach of children.
Do not use Levobupivacaine after the expiry date which is stated on the label. The expiry date refers to the last day of that month.
Your doctor will store this medicine for you.
The solution should be used immediately after opening.
Do not use this medicine if there are visible particles in it.
This medicinal product does not require any special storage conditions.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
6. Contents of the pack and other information
What Levobupivacaine contains
The active substance is levobupivacaine (as levobupivacaine hydrochloride).
Levobupivacaine 2.5 mg/ml solution for injection/infusion: 1 ml solution contains 2.5 mg levobupivacaine (as levobupivacaine hydrochloride). Each ampoule of 10ml contains 25 mg levobupivacaine (as levobupivacaine hydrochloride).
Levobupivacaine 5 mg/ml solution for injection/infusion: 1 ml solution contains 5 mg levobupivacaine (as levobupivacaine hydrochloride). Each ampoule of 10ml contains 50mg levobupivacaine (as levobupivacaine hydrochloride).
The other ingredients are water for injection, sodium chloride, and small quantity of sodium hydroxide and hydrochloric acid.
This medicine contains an excipient with known effect (sodium). See section 2 for further information.
pH 4.0-6.0
Osmolarity: 271-372 mOsmol/l
What Levobupivacaine looks like and contents of the pack
This medicine is a clear, colourless solution, in polypropylene ampoules in sterile blister pack. Each ampoule contains 10 ml of solution. It is supplied in packs of 5, 10 or 20 ampoules.
Not all pack sizes may be marketed.
Marketing Authorisation Holder and Manufacturer
Fresenius Kabi Limited,
Cestrian Court,
Eastgate Way,
Manor Park,
Runcorn,
Cheshire WA71NT United Kingdom
Fresenius Kabi Deutschland GmbH D-61346 Bad Homburg v.d.H.
Germany
This leaflet was last revised in 03/2014
The following information is intended for medical or health care professionals only: Levobupivacaine 2.5 mg/ml or 5.0 mg/ml solution for injection/infusion.
Instructions for use and handling
Levobupivacaine 2.5mg/ml or 5.0mg/ml solution for injection/infusion is intended for single use
V001
Levobupivacaine®
(levobupivacaine)
2.5 mg/ml and 5.0 mg/ml
Read the label carefully. Shake down any contents from the neck.
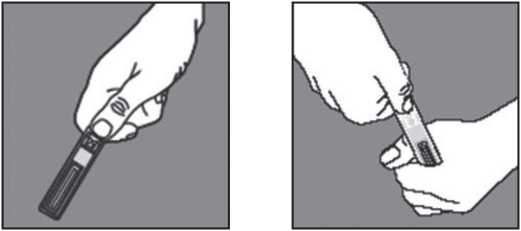



Push firmly the tapered luer tip of syringe into ampoule.
Gently push the ampoule towards you with the forefinger and withdraw the content slowly, taking special care at first.
Hold ampoule in palm of hand waist height. Hold arrow on ampoule held between thumb and forefinger (thumb away from you). Twist quickly and sharply towards you (anti-clockwise).

FRESENIUS
KABI
01-59-12-xxx
V001