Octanate 50 Iu/Ml Powder And Solvent For Solution For Injection
SUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
Octanate 50 IU/ml
Powder and solvent for solution for injection
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
Octanate 50 IU/ml contains nominally either 250 IU or 500 IU human coagulation factor VIII per vial.
The product contains approximately 50 IU* per ml human coagulation factor VIII when reconstituted with the supplied solvent (5 ml for 250 IU/vial and 10 ml for 500 IU/vial).
The product contains approximately < 30 IU per ml von Willebrand factor (VWF:RCo).
This medicinal product contains less than 1 mmol sodium (23 mg) per dose, i.e. essentially 'sodium-free' for 250 IU/vial and contains up to 1.75 mmol sodium (40 mg) per dose for 500 IU/vial. To be taken into consideration by patients on a controlled sodium diet.
For the full list of excipients, see section 6.1.
*The potency (IU) is determined using the European Pharmacopoeia chromogenic assay. The mean specific activity of Octanate is > 100 IU/mg protein.
3 PHARMACEUTICAL FORM
Powder and solvent for solution for injection.
The powder is white or pale yellow, also appearing as a friable solid. The solvent is a clear, colourless liquid.
CLINICAL PARTICULARS
4
4.1 Therapeutic indications
Treatment and prophylaxis of bleeding in patients with haemophilia A (congenital factor VIII deficiency)
This preparation does not contain von Willebrand factor in pharmacologically effective quantities and is therefore not indicated in von Willebrand’s disease.
4.2 Posology and method of administration
Treatment should be initiated under the supervision of a physician experienced in the treatment of haemophilia.
Posology
The dosage and duration of the substitution therapy depend on the severity of the factor VIII deficiency, on the location and extent of the bleeding, and on the patient’s clinical condition.
The number of units of factor VIII administered is expressed in International Units (IU), which are related to the current World Health Organisation (WHO) international standard for factor VIII products. Factor VIII activity in plasma is expressed either as a percentage (relative to normal human plasma) or in International Units (relative to an International Standard for factor VIII in plasma).
One International Unit (IU) of factor VIII activity is equivalent to that quantity of factor VIII in one ml of normal human plasma. The calculation of the required dosage of factor VIII is based on the empirical finding that 1 IU factor VIII per kg body weight raises the plasma factor VIII activity by 1.5 % to 2 % of normal. The required dosage is determined using the following formula:
Required units = body weight (kg) x desired factor VIII rise (%) (IU/dl) x 0.5
The amount and frequency of administration should always be adjusted according to the clinical effectiveness in the individual patient.
In the case of the following haemorrhagic events, the factor VIII activity should not fall below the given plasma activity level (in % of normal) in the corresponding period. The following table can be used to guide dosing in bleeding episodes and surgery:
|
Degree of haemorrhage/ Type of surgical procedure |
F actor VIII level required (%) (IU/dl) |
Frequency of doses (hours) / Duration of therapy (days) |
|
Haemorrhage | ||
|
Early haemarthrosis, muscle bleeding or oral bleeding |
20 - 40 |
Repeat every 12 to 24 hours. At least 1 day, until the bleeding episode as indicated by pain is resolved or healing is achieved. |
|
More extensive haemarthrosis, muscle bleeding or haematoma |
30 - 60 |
Repeat infusion every 12 to 24 hours for 3 to 4 days or more until pain and disability are resolved. |
|
Life-threatening haemorrhages |
60 - 100 |
Repeat infusion every 8 to 24 hours until threat is resolved. |
|
Surgery | ||
|
Minor including tooth extraction |
30 - 60 |
Every 24 hours, at least 1 day, until healing is achieved. |
|
Major |
80 - 100 (pre- and postoperative) |
Repeat infusion every 8 to 24 hours until adequate wound healing, then therapy for at least another 7 days to maintain a FVIII activity of 30% to 60%. |
During the course of treatment, appropriate determination of factor VIII levels is advised to guide the dose to be administered and the frequency of repeated infusions. In the case of major surgical interventions in particular, a precise monitoring of the substitution therapy by means of coagulation analysis (plasma factor VIII activity) is indispensable. Individual patients may vary in their response to factor VIII, achieving different levels of in vivo recovery and demonstrating different half-lives.
For long-term prophylaxis against bleeding in patients with severe haemophilia A, the usual doses are 20 to 40 IU of factor VIII per kg body weight at intervals of 2 to 3 days.
Paediatric population
A clinical study which was conducted in 15 patients of 6 years of age or less did not identify any special dosage requirements for children.
Clinical data on the use of Octanate in previously untreated patients (PUPs) are limited (see section 4.8).
Patients should be monitored for the development of factor VIII inhibitors. If the expected factor VIII activity plasma levels are not attained, or if bleeding is not controlled with an appropriate dose, an assay should be performed to determine if a factor VIII inhibitor is present. In patients with high levels of inhibitor, factor VIII therapy may not be effective and other therapeutic options should be considered. Management of such patients should be directed by physicians with experience in the care of patients with haemophilia. See also 4.4.
Method of administration
For instructions on reconstitution of the medicinal product before administration, see section 6.6. The product should be administered via the intravenous route. It is recommended not to administer more than 2 - 3 ml per minute.
4.3
Contraindications
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
4.4 Special warnings and precautions for use
• As with any intravenous protein product, allergic type hypersensitivity reactions are possible. The product contains traces of human proteins other than factor VIII. Patients should be informed of the early signs of hypersensitivity reactions including hives, generalised urticaria, tightness of the chest, wheezing, hypotension, and anaphylaxis. If these symptoms occur, they should be advised to discontinue use of the product immediately and contact their physician.
In case of shock, standard medical treatment of shock should be implemented.
• The formation of neutralising antibodies (inhibitors) to factor VIII is a known complication of the treatment of individuals with haemophilia A. These inhibitors are usually IgG immunoglobulins directed against the factor VIII procoagulant activity, which are quantified in Bethesda Units (BU) per ml of plasma using the modified assay. The risk of developing inhibitors is correlated to the exposure to anti-haemophilic factor VIII, this risk being highest within the first 20 exposure days. Rarely, inhibitors may develop after the first 100 exposure days. Patients treated with human coagulation factor VIII should be carefully monitored for the development of inhibitory antibodies by appropriate clinical observations and laboratory test. See also 4.8. Undesirable effects
• There have been reports in the literature showing a relationship between the occurrence of a factor VIII inhibitor and allergic reactions. Therefore, if allergic reactions occur, the patient should be examined for the presence of an inhibitor. Patients with factor VIII inhibitors may be at an increased risk of anaphylaxis with subsequent treatment with factor VIII. Consequently, the first administration of factor VIII should, according to the treating physician’s judgement, be performed under medical supervision where appropriate medical care for allergic reactions can be provided.
• Standard measures to prevent infections resulting from the use of medicinal products prepared from human blood or plasma include selection of donors, screening of individual donations and plasma pools for specific markers of infection and the inclusion of effective manufacturing steps for the inactivation/removal of viruses. Despite this, when medicinal products prepared from human blood or plasma are administered, the possibility of transmitting infective agents cannot be totally excluded. This also applies to unknown or emerging viruses and other pathogens.
The measures taken are considered effective for enveloped viruses such as HIV, HBV and HCV, and for the non-enveloped virus HAV. The measures taken may be of limited value against non-enveloped viruses such as parvovirus B19. Parvovirus B19 infection may be serious for pregnant women (foetal infection) and for individuals with immunodeficiency or increased erythropoiesis (e.g. hemolytic anaemia).
Appropriate vaccination (hepatitis A and B) should be considered for patients in regular/repeated receipt of human plasma-derived factor VIII products.
It is strongly recommended that every time Octanate is administered to a patient, the name and batch number of the product are recorded in order to maintain a link between the patient and the batch of the product.
4.5 Interaction with other medicinal products and other forms of interaction
No interaction studies have been performed.
There are no known interactions of human coagulation factor VIII products with other medicinal products.
4.6 Pregnancy and lactation
There is no or limited amount of data from the use of Octanate in pregnant women.
Animal reproduction studies have not been conducted with factor VIII. Based on the rare occurrence of haemophilia A in women, experience regarding the use of factor VIII during pregnancy and breast-feeding is not available. Therefore, factor VIII should be used during pregnancy and lactation only if clearly indicated.
4.7 Effects on ability to drive and use machines
Octanate has no or negligible influence on the ability to drive and use machines.
4.8 Undesirable effects
• Hypersensitivity or allergic reactions (which may include angiooedema, burning and stinging at the infusion site, chills, flushing, generalised urticaria, headache, hives, hypotension, lethargy, nausea, restlessness, tachycardia, chest tightness, tingling, vomiting, wheezing) have been observed infrequently, and may in some cases progress to severe anaphylaxis (including shock).
• On rare occasions, fever has been observed.
• Patients with haemophilia A may develop antibodies (inhibitors) to factor VIII. If such inhibitors occur, the condition will manifest as an insufficient clinical response. In such cases, it is recommended that a specialised haemophilia centre be contacted.
In an ongoing clinical trial in previously untreated patients (PUPs), 3 out of 39 (7.6%) PUPs treated with Octanate on-demand developed inhibitors with a titre above 5 BU. One patient developed inhibitors with a titre below 5 BU. Two cases (5.1%) were of clinical relevance; the remaining two subjects displayed inhibitors that disappeared spontaneously without an Octanate dose change. All inhibitors developed with on-demand treatment and before exposure day 50.
35 PUPs had a baseline FVIII activity < 1% and 4 PUPs had <2% FVIII:C. At the time point of the interim analysis, there were 34 patients who had already 20 or more exposure days to Octanate and 30 patients with 50 or more exposure days to Octanate. No inhibitors were observed in PUPs receiving prophylaxis with Octanate. During the study, 12 PUPs underwent 14 surgical procedures. The median age at the first exposure was 7 months (range 3 days to 67 months). The median number of exposure days in the clinical trial was 100 (range 1-553).
|
System Organ Class |
Rare |
Very rare |
|
Immune system disorders |
hypersensitivity reaction |
anaphylactic shock |
|
General disorders and administration site conditions |
fever |
rare (>1/10,000 to <1/1,000) very rare (<1/10,000)
• For information on viral safety see 4.4.
4.9 Overdose
No case of overdose has been reported.
5 PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: antihemorrhagics: blood coagulation factor VIII ATC-Code: B02BD02
The factor VIII/ von Willebrand factor complex consists of two molecules (FVIII and vWF) with different physiological functions. When infused into a haemophiliac patient, factor VIII binds to von Willebrand factor in the patient’s circulation.
Activated factor VIII acts as a cofactor for activated factor IX, accelerating the conversion of factor X to activated factor X. Activated factor X converts prothrombin into thrombin. Thrombin then converts fibrinogen into fibrin and a clot can be formed.
Haemophilia A is a sex-linked hereditary disorder of blood coagulation due to decreased levels of factor VIII:C and results in profuse bleeding into joints, muscles, or internal organs, either spontaneously or as a results of accidental or surgical trauma. By replacement therapy the plasma levels of factor VIII are increased, thereby enabling a temporary correction of the factor deficiency and correction of the bleeding tendencies.
Octanate is being assessed for induction of immune tolerance induction (ITI) therapy in an ongoing observational clinical study.
In an interim analysis of the 69 patients so far treated with Octanate via ITI, 49 patients have completed the study. In the patients where the inhibitor was successfully eliminated, the monthly bleeding rates were significantly reduced.
5.2 Pharmacokinetic properties
Human plasma coagulation factor VIII (from the powder) is a normal constituent of the human plasma and acts like the endogenous factor VIII. After injection of the product, approximately two-thirds to three-quarter of the factor VIII remain in the circulation. The level of factor VIII activity reached in the plasma should be between 80% - 120% of the predicted factor VIII activity.
Plasma factor VIII activity decreases by a two-phase exponential decay. In the initial phase, distribution between the intravascular and other compartments (body fluids) occurs with a half-life of elimination from the plasma of 3 to 6 hours. In the subsequent slower phase (which probably reflects the consumption of factor VIII), the
half-life varies between 8 to 20 hours, with an average of 12 hours. This corresponds to the true biological half-life.
For Octanate the following results were achieved for two pharmacokinetic studies with 10 and 14 haemophilia A patients, respectively:
|
Recovery (% x IU-1 x kg) |
AUC*norm (% x h x IU-1 x kg) |
Half-life (h) |
MRT* (h) |
Clearance (ml x h-1 x kg) | |
|
Study 1, n = 10 Mean ± SD* |
2.4 + 0.36 |
45.5 + 17.2 |
14.3 + 4.01 |
19.6 + 6.05 |
2.6 + 1.21 |
|
Study 2, n = 14 Mean ± SD* |
2.4 + 0.25 |
33.4 + 8.50 |
12.6 + 3.03 |
16.6 + 3.73 |
3.2 + 0.88 |
AUC* = area under the curve, MRT* = mean residence time, SD* = standard deviation
5.3 Preclinical safety data
Toxicological data available on tri-n-butylphosphate (TNBP) and polysorbate 80
(tween 80), the solvent/detergent reagents used in the SD method of viral inactivation during manufacture of Octanate, although limited for the latter, indicate that adverse effects are unlikely at the anticipated human exposures.
Even doses of several times the recommended human dosage per kilogram body weight of these reagents show no toxic effects on laboratory animals. No mutagenic potential was observed for either of the two substances.
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
Powder:
• Sodium citrate
• Sodium chloride
• Calcium chloride
• Glycine
Solvent: Water for injections
6.2 Incompatibilities
mixed
failure to the
In the absence of compatibility studies, this medicinal product must not be with other medicinal products.
Only the provided injection or infusion sets should be used, because treatment can occur as a consequence of human coagulation factor VIII adsorption internal surface of some injection/infusion equipment.
6.3 Shelf life
2 years
The reconstituted solution must be used immediately and on one occasion only.
6.4 Special precautions for storage
Store in a refrigerator (2°C - 8°C).
Do not freeze.
Keep the vials in the outer carton in order to protect from light.
For storage conditions after reconstitution of the medicinal product, see section 6.3.
6.5 Nature and contents of container
One package Octanate contains:
- Powder in a vial (type I glass), with a stopper (chlorobutyl or bromobutyl rubber), and a flip off cap
- solvent in a vial (type I glass), with a stopper (chlorobutyl or bromobutyl rubber), and a flip off cap
- one disposable syringe, one transfer set Mix2VialTM, one injection needle, and two alcohol swabs.
The two available pack sizes differ in the amount of human blood coagulation factor VIII/ solvent:
250 IU/vial: reconstitution with 5 ml 500 IU/vial: reconstitution with 10 ml
Not all pack sizes may be marketed.
6.6 Special precautions for disposal
• Please read all the instructions and follow them carefully!
• Do not use Octanate after expiry date given on the label.
• During the procedure described below, sterility must be maintained!
• The solution in the syringe should be clear or slightly pearly shimmery. Do not inject solutions that are cloudy or have deposits.
• Use the prepared solution immediately, to prevent microbial contamination.
• Only use the injection set provided. The use of other injection/infusion equipment can cause additional risks and treatment failure.
Instructions for preparing the solution:
1. Do not use the product directly from the refrigerator. Allow the solvent and the powder in the closed vials to reach room temperature.
2. Remove the flip off caps from both vials and clean the rubber stoppers with one of the provided alcohol swabs.
3. The Mix2vial™ is depicted in Fig. 1. Place the solvent vial on an even surface and hold it firmly. Take the Mix2Vial™ and turn it upside down. Place the blue part of the Mix2Vial™ on top of the solvent vial and press firmly down until it snaps (Fig. 2+3).
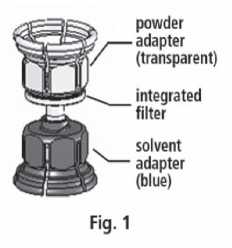


Fig. 3

4. Place the powder vial on an even surface and hold it
firmly. Take the solvent vial with the attached Mix2Vial™ and turn it upside down. Place the transparent part on top of the powder vial and press firmly down until it snaps (Fig. 4). The solvent flows automatically into the powder vial.

5. With both vials still attached, gently swirl the powder vial until the product is dissolved.
The dissolving is completed in less than 10 minutes at room temperature. Slight foaming might occur during preparation. Unscrew the Mix2Vial™ into two parts (Fig. 5). Foaming will disappear.
Dispose the empty solvent vial with the blue part of the Mix2Vial™.
Instructions for injection:
As a precaution, your pulse rate should be taken before and during the injection. If a marked increase in your pulse rate occurs, reduce the injection speed or interrupt the administration for a short time.
1. Attach the syringe to the transparent part of the Mix2Vial™. Turn the vial upside down and draw the solution into the syringe (Fig. 6).
The solution in the syringe should be clear or slightly pearly shimmery. Once the solution has been transferred, firmly hold the plunger of the syringe (keeping it facing down) and remove the syringe from the Mix2Vial™ (Fig. 7). Dispose the Mix2Vial™ and the empty vial.


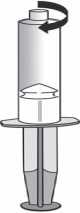
Fig. 7
2. Clean the chosen injection site with one of the provided alcohol swabs.
3. Attach the provided injection needle to the syringe
4. Insert the injection needle into the chosen vein. If you have used a tourniquet to make the vein easier to see, this tourniquet should be released before you start injecting Octanate.
No blood must flow into the syringe due to the risk of formation of fibrin clots.
5. Inject the solution into the vein at a slow speed, not faster than 2-3 ml per minute.
If you use more than one vial of Octanate powder for one treatment, you may use the same injection needle and syringe again. The Mix2Vial™ is for single use only.
Any unused medicinal product or waste material should be disposed of in accordance with local requirements.
7 MARKETING AUTHORISATION HOLDER
Octapharma Ltd The Zenith Building,
26 Spring Gardens Manchester M2 1AB United Kingdom
8 MARKETING AUTHORISATION NUMBER(S)
PL 10673/0018
9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
28/07/2010
10 DATE OF REVISION OF THE TEXT
13/06/2013