Ovestin Cream
Out of date information, search anotherAssessed against UK PIL dated November 2005
OVESTIN® CREAM ESTRIOL 0.1% W/W CREAM (estriol)
PATIENT INFORMATION LEAFLET
Your medicine is available using either of the above names, but will be referred to as Ovestin Cream throughout this leaflet.
Please read this leaflet carefully before you start taking this medicine.
WHAT YOU SHOULD KNOW ABOUT YOUR MEDICINE
This leaflet has been written to help you use your medicine properly.
If you have any questions or worries, ask your doctor or a pharmacist.
At the end of the leaflet you will find a list of things to remember about your medicine.
Keep the leaflet until you have finished your medicine. You may want to read it again.
WHAT IS OVESTIN CREAM?
Each gram contains 1mg of the active ingredient Estriol.
It also contains chlorhexidine hydrochloride, eutanol G, cetyl palmitate, glycerin, cetyl alcohol, stearyl alcohol, polysorbate 60, sorbitan monostearate, lactic acid, sodium hydroxide and purified water.
Ovestin Cream is a white smooth cream.
Each tube contains 15g of cream.
Ovestin Cream is one of a group of medicines called Hormone Replacement Therapy (HRT).
Manufactured by: Organon (Ireland) Ltd, Swords, Ireland.
Procured from within the EU and repackaged by: Doncaster Pharmaceuticals Group Ltd, Kirk Sandall, Doncaster, DN3 1QR
Product Licence holder: BR Lewis Pharmaceuticals Ltd, Kirk Sandall, Doncaster,
DN31QR _
POM PL No: 08929/0342
WHAT IS OVESTIN CREAM USED FOR?
Ovestin Cream is used to treat vaginal complaints that are caused by having too little estrogen.
It can also be used before or after vaginal surgery.
BEFORE YOU USE THE CREAM
Some women shouldn’t use Ovestin Cream Before you are given the cream, read these questions.
• Are you pregnant or breast-feeding?
• Have you had angina or myocardial infarction?
• Have you had a thrombosis (a blood clot)?
• Have you had breast cancer?
• Have you had cancer of other sex organs?
• Do you have porphyria (a rare metabolic disorder)?
• Have you had an allergic reaction to any of the ingredients in Ovestin Cream?
If the answer to any of these questions is YES:
You should NOT use the cream.
• Have you had unusual growth of the lining of the womb (endometrial hyperplasia)?
• Have you had unexplained vaginal bleeding?
• Have you had liver disease?
If the answer to any of these questions is YES:
> Did you tell your doctor at the last visit or an earlier visit?
If you did NOT then you should do so as soon as possible and before using the cream. Even so, your doctor may still want you to use it.
This medicine contains cetyl alcohol and stearyl alcohol which may cause local skin reactions (e.g. contact dermatitis).
SAFETY OF HRT
As well as benefits, HRT has some risks, which you need to consider when you’re deciding whether to take it, or whether to carry on taking it.
MEDICAL CHECK-UPS
Before you start taking HRT, your doctor should ask about your own and your family’s medical history. Your doctor may decide to examine your breasts and/or your abdomen, and may do an internal examination — but only if these examinations are necessary for you or if you have any special concerns. Once you’ve started on HRT, you should see your doctor for regular check-ups (at least once a year). At these check-ups, your doctor may discuss with you the benefits and risks of continuing to take HRT.
Be sure to:
• go for regular breast screening and cervical smear tests
• regularly check your breasts for any changes such as dimpling of the skin, changes in the nipple, or any lumps you can see or feel
SOME WOMEN NEED SPECIAL CARE
Special care by your doctor may be necessary in some cases.
> Tell your doctor if you have ever had:
• any disease of the heart or circulation;
• blood clots;
• relatives who have had blood clots;
• a rare disease called systemic lupus erythematosus;
• high blood pressure;
• migraine headaches;
• epilepsy;
• fibroids;
• gallstones;
• asthma;
• too much cholesterol or other fatty substances in the blood;
• deafness caused by thickened ear tissue;
• kidney disease;
• endometriosis;
• diabetes.
EFFECTS ON YOUR HEART OR CIRCULATION Heart disease
HRT is not recommended for women who have heart disease, or have had heart disease recently.
If you have ever had heart disease, talk to your doctor to see if you should be taking HRT.
HRT will not help to prevent heart disease.
Studies with one type of HRT (containing conjugated estrogen plus the progestagen MPA) have shown that women may be slightly more likely to get heart disease during the first year of taking the medication. For other types of HRT, the risk is likely to be similar, although this is not yet certain.
If you get:
• a pain in your chest that spreads to your arm or neck, see a doctor as soon as possible and do not use any more HRT until a doctor says you can. This pain could be a sign of heart disease.
Stroke
Recent research suggests that HRT slightly increases the risk of having a stroke. Other things that can increase the risk of stroke include:
• getting older
• high blood pressure
• smoking
• drinking too much alcohol
• an irregular heartbeat
If you are worried about any of these things, or if you have had a stroke in the past, talk to your doctor to see if you should take HRT.
Compare
Looking at women in their 50s who are not taking HRT — on average, over a 5-year period, 3 in 1000 would be expected to have a stroke. For women in their 50s who are taking HRT, the figure would be 4 in 1000. Looking at women in their 60s who are not taking HRT — on average, over a 5-year period, 11 in 1000 would be expected to have a stroke. For women in their 60s who are taking HRT, the figure would be 15 in 1000.
If you get:
• unexplained migraine-type headaches, with or without disturbed vision See a doctor as soon as possible and do not use any more HRT until a doctor says you can. These headaches may be an early warning sign of a stroke.
Blood clots
HRT may increase the risk of blood clots in the veins (also called deep vein thrombosis or DVT), especially during the first year of taking it. These blood clots are not always serious, but if one travels to the lungs, it can cause chest pain, breathlessness, collapse, or even death. This condition is called pulmonary embolism, or PE. DVT and PE are examples of a condition called venous thromboembolism, or VTE.
You are more likely to get a blood clot:
• if you are seriously overweight
• if you have had a blood clot before
• if any of your close family have had blood clots
• if you have had one or more miscarriages
• if you have any blood clotting problem that needs treatment with a medicine such as warfarin
• if you’re off your feet for a long time because of major surgery, injury or illness
• if you have a rare condition called SLE
If any of these things apply to you, talk to your doctor to see if you should take HRT.
Compare
Looking at women in their 50s who are not taking HRT — on average, over a 5-year period, 3 in 1000 would be expected to get a blood clot. For women in their 50s who are taking HRT, the figure would be 7 in 1000. Looking at women in their 60s who are not taking HRT — on average, over a 5-year period, 8 in 1000 would be expected to get a blood clot. For women in their 60s who are taking HRT, the figure would be 17 in 1000.
If you get:
• painful swelling in your leg
• sudden chest pain
• difficulty breathing
> See a doctor as soon as possible and do not use any more HRT until a doctor says you can. These may be signs of a blood clot. If you’re going to have surgery, make sure your doctor knows about it. You may need to stop using HRT about 4 to 6 weeks before the operation, to reduce the risk of a blood clot. Your doctor will tell you when you can start taking HRT again.
EFFECTS ON YOUR RISK OF DEVELOPING CANCER
Breast cancer
Women who have breast cancer, or have had breast cancer in the past, should not take HRT.
Taking HRT slightly increases the risk of breast cancer; so does having a later menopause. The risk for a postmenopausal woman taking estrogen-only HRT for 5 years is about the same as for a woman of the same age who’s still having periods over that time and not taking HRT. The risk for a woman who is taking estrogen plus progestagen HRT is higher than for estrogen-only HRT (but estrogen plus progestagen HRT is beneficial for the endometrium).
For all kinds of HRT, the extra risk of breast cancer goes up the longer you take it, but returns to normal within about 5 years after stopping HRT. Your risk of breast cancer is also higher:
• if you have a close relative (mother, sister or grandmother) who has had breast cancer
• if you are seriously overweight
AMEND AT PRINT 'add bullet point
Compare
Looking at women aged 50 who are not taking HRT — on average, 32 in 1000 will be diagnosed with breast cancer by the time they reach the age of 65. For women who start taking estrogen-only HRT at age 50 and take it for 5 years, the figure will be between 33 and 34 in 1000 (ie an extra 1-2 cases). If they take estrogen-only HRT for 10 years, the figure will be 37 in 1000 (ie an extra 5 cases).
If you notice:
any changes in your breast, such as:
• dimpling of the skin
• changes in the nipple
• any lumps you can see or feel
> Make an appointment to see your doctor as soon as possible.
Endometrial cancer (cancer of the lining of the womb)
Taking estrogen-only HRT tablets for a long time can increase the risk of developing cancer of the lining of the womb (the endometrium). It is possible there may be a similar risk with estrogen cream used directly in the vagina for repeated treatments or over along time. You do not need to take a separate progestagen with Ovestin Cream, but - If you get: breakthrough bleeding or spotting, it’s usually nothing to worry about, but you should
> Make an appointment to see your doctor. It could be a sign that your endometrium has become thicker.
Ovarian cancer
Ovarian cancer (cancer of the ovaries) is very rare, but it is serious. It can be difficult to diagnose, because there are often no obvious signs of the disease. Some studies have indicated that taking estrogen-only HRT for more than 5 years may increase the risk of ovarian cancer. It is not yet known whether other kinds of HRT increase the risk in the same way.
WHAT OTHER MEDICINES ARE YOU TAKING?
Other medicines may effect how Ovestin Cream works or it may effect how they work. These include medicines to treat epilepsy (eg phenobarbital, phenytoin, carbamezapine), infectious diseases (eg rifampicin, rifabutin, nevirapine, efavirenz, ritonavir, nelfinavir) and St John’s wort.
> Tell your doctor if you are taking (or intend to take) any other medicines. If you have a vaginal infection, your doctor may also
prescribe a medicine to treat the infection.
HOW DO I USE OVESTIN CREAM?
It is important to use this medicine only as directed by your doctor or pharmacist. If you have had your womb and ovaries removed, you can start using your medicine straight away. If you have never used HRT before or if you are changing over from a period-free HRT, you can also use your medicine straight away.
If you are changing over from another type of HRT where you have a period, start taking your medicine one week after you finish the other HRT.
HOW MUCH?
For vaginal complaints the usual dose is 1 applicator dose (0.5mg Estriol in 0.5g of cream) a day for the first 2 to 3 weeks. Then the dose is 1 applicator-dose twice a week. Your doctor will prescribe the lowest dose that relieves your symptoms. Your doctor may want you to stop from time to time (every 2 to 3 months for a period of 4 weeks), to check if you still need treatment. Before vaginal surgery the dose is 1 applicator-dose (0.5mg Estriol in 0.5g of cream) a day for 2 weeks before the operation. After the operation, do not use the cream again for at least 2 weeks and then use 1 applicator-dose twice a week. Keep using this medicine as prescribed by your doctor. Do not stop just because you seem to be better. If you stop too early or too suddenly your complaints may return.
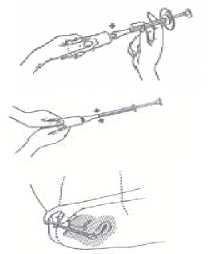
HOW TO APPLY THE CREAM
Use the applicator to apply the cream in the vagina. It is a good idea to do this before going to bed. One application contains 0.5mg of Estriol.
1. Remove cap from the tube, invert it, and use the sharp point to open the tube.
2. Screw the end of the applicator onto the tube.
3. Squeeze tube to fill the applicator with the cream until the plunger stops (at the ring mark).
4. Unscrew applicator from tube and replace cap on tube.
5. To apply the cream, lie down, insert the end of the applicator deep into the vagina and slowly push plunger all the way in.
After use, pull the plunger out of the barrel. Wash the plunger and barrel in hand hot, soapy water. Do not use detergents. Rinse well with clean water afterwards.
DO NOT PUT THE APPLICATOR IN BOILING WATER.
WHAT ABOUT SIDE EFFECTS?
Serious side effects are rare.
> See your doctor if any of the following occur - your doctor may decide to stop giving you the cream:
• If your blood pressure increases significantly
• If you suddenly develop migraine-type headaches
• If your skin goes yellow (jaundice)
• If you develop blood clots (see above)
If you develop any of the other conditions that are listed in the Section on "Before you use the cream". Less serious side effects sometimes occur in some people. These usually settle down during treatment as the body adjusts to the medicine.
If you have any of these following side effects, tell your doctor. He may decide to stop your treatment for a while.
• Irritation or itching of the skin in or around the vagina
• You may notice an increased vaginal discharge
• Some people may have gall bladder disease
• You may have skin problems such as a rash or an allergy to the sun.
• You may notice some vaginal spotting or bleeding
• Sometimes the breasts become swollen, tender or painful
• Very occasionally headaches occur
• Some people may feel sick or be sick
Dementia: HRT will not prevent memory loss. In one study of women who started using combined HRT after the age of 65, a small increase in the risk of dementia was observed.
> Tell your doctor about any problems that you think might be caused by the cream.
HOW SHOULD YOU STORE THIS MEDICINE?
• Do not use this medicine after the expiry date printed on the carton and tube.
• Store the cream at room temperature (15-25°C).
• KEEP ALL MEDICINES OUT OF THE REACH AND SIGHT OF CHILDREN
GENERAL THINGS TO REMEMBER ABOUT YOUR MEDICINES
1. This medicine has been prescribed for your current medical problems. Do not use it for other medical problems.
2. Do not allow other people to use your medicines and do not use medicines meant for other people.
3. Tell any doctor treating you what medicines you are taking. Always carry a medical information card stating which medicines you are using. This can also be very important in case you are involved in an accident.
4. Return unused medicines to the pharmacy for disposal.
5. Make sure that other people you may live with or who look after you read this information.
6. If your cream appears discoloured, or shows any other signs of deterioration, take it to your pharmacist who will advise you.
MORE ABOUT OVESTIN CREAM
Ovestin Cream contains synthetic Estriol, one of the female sex hormones (estrogens). Estrogens are produced in the ovaries. They cause sexual development in women and control the menstrual cycle during the childbearing years. When women get older the ovaries gradually produce less estrogen. This happens at the menopause (usually around the age of 50). If the ovaries are removed surgically (ovariectomy) before the menopause, estrogen production stops very suddenly. Shortage of estrogens may cause the vaginal wall to become thin and dry. So sexual intercourse may become painful and vaginal infections may occur. These complaints can be relieved by using medicines containing estrogen. However it may take several days or weeks before you notice an improvement.
Ovestin Cream may also be prescribed to help wound healing after vaginal surgery. Ovestin Cream usually does not cause vaginal bleeding. Ovestin Cream is easy to remove with water.
Leaflet issue and revision date (Ref): 21.03.06.
Ovestin® is a registered trademark of N.V.Organon.
WHAT TO DO IF OVESTIN CREAM IS SWALLOWED ACCIDENTALLY OR IF TOO MUCH IS TAKEN AT ONE TIME
If someone has swallowed some cream by accident, or too much cream is applied at any time, there is no need to worry. However, you should consult a doctor. The person may feel sick or be sick. Women may have some vaginal bleeding after a few days.
WHAT IF I MISS A DOSE?
Apply the missed dose when you remember, unless you are more than 12 hours late. If you are more than 12 hours late just skip the missed dose.