Qvar 100 Autohaler
Patient Information Leaflet Qvar™ 100 Autohaler™
(beclometasone dipropionate)
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
This medicine is known by the above name but will be referred to as Qvar Autohaler throughout the remainder of this leaflet.
What is in this leaflet
1. What Qvar Autohaler is and what it is used for
2. What you need to know before you use Qvar Autohaler
3. How to use Qvar Autohaler
4. Possible side effects
5. How to store Qvar Autohaler
6. Contents of the pack and other information
1. What Qvar Autohaler is and what it is used for
Qvar Autohaler contains beclometasone dipropionate, which is one of a group of medicines known as corticosteroids.
Qvar Autohaler is used to prevent the symptoms of mild, moderate, or severe asthma in patients who require regular treatment.
How your medicine works
• Qvar Autohaler works deep in your lungs to make breathing easier by reducing the inflammation, swelling and irritation in the airways. This type of medicine is known as a ‘preventer’. It needs to be taken regularly every day, even if you have no symptoms.
• This inhaler will not give immediate relief of wheezing or breathlessness during a sudden asthma attack. You will need to use a ‘reliever’ inhaler, which contains a different medicine. You should still continue to use this inhaler.
2. Before you use Qvar Autohaler DO NOT use Qvar Autohaler if you:
• are allergic (hypersensitive) to beclometasone dipropionate or any of the other ingredients of this medicine (listed in section 6).
• are suffering from a sudden attack of breathlessness. It will not help. Use a quick-acting ‘reliever’ inhaler for this purpose and carry it with you at all times.
Warnings and precautions
Talk to your doctor before you start to use this
medicine if:
• you are suffering from tuberculosis (TB) now or have suffered from it in the past
• you are allergic to other similar inhalers
• you must avoid alcohol for any reason
• your asthma seems to be getting worse. Perhaps you are more wheezy and short of breath than usual, your ‘reliever’ inhaler seems to be less effective, you require more puffs from your ‘reliever’ inhaler than usual, or you do not seem to be getting better. Your doctor may need to increase the dose of your steroid inhaler or give you a course of steroid tablets, or change your treatment altogether. If you have an infection in your chest your doctor may prescribe a course of antibiotics.
• when transferring from steroid tablets to an inhaler you find that, even if your chest is getting better, you feel generally unwell, you develop a rash, eczema or a runny nose and sneezing (rhinitis). Do not stop treatment with your inhaler unless your doctor tells you to.
Important points to remember while you are using this
medicine:
• Your doctor may prescribe this inhaler to replace steroid tablets, which may mean that for a short time you have to take both medicines.
It is important to follow your doctor’s advice. Whilst you are reducing the number of steroid tablets that you take you may feel generally unwell even though you can breathe as well as normal or better. If you have other allergies you may find that stopping your steroid tablets makes them worse. If this happens keep using your inhaler and tell your doctor.
• If you have been treated for a long time with high doses of inhaled steroid, you may require a course of steroid tablets or possibly a steroid injection in times of stress. For example, during admission to hospital after a serious accident, before an operation, during an acute attack of asthma or if you have a chest infection or other serious illness. Your doctor will decide if you need any extra steroid treatment and will also advise you as to how long you need to take the course of steroid tablets and how you should reduce these as you get better.
• There may be times when you need to take steroid tablets as well as using your inhaler, for example if you have worsening asthma attacks, you get a chest infection or you need an operation. Your doctor may give you a small supply of steroid tablets to be taken in these situations; if he does you will be given full instructions on how and when to take them. Contact your doctor immediately if you think that you need to take steroid tablets, even if you have your own supply.
• You should have been given a steroid card with this inhaler; if you have not, please ask your pharmacist for one. Make sure you carry your steroid card with you at all times until your doctor decides that it is no longer necessary.
• Visit your doctor regularly for a review of your condition.
• If you have to go into hospital, remember to take all your inhalers and other medicines with you.

Other medicines and Qvar Autohaler
• Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including any medicines bought without a prescription.
In particular tell your doctor if you are taking:
• Disulfiram
• Metronidazole
Pregnancy and breast-feeding
• If you are pregnant, planning to become pregnant or are breast-feeding, ask your doctor for advice before taking this medicine.
Driving and using machines
• Qvar Autohaler is not known to affect your ability to drive or operate machinery.
Important information about some of the ingredients of Qvar:
• Qvar contains a small amount of alcohol
3. How to use Qvar Autohaler
There are two strengths of the Qvar Autohaler device available and your doctor will have chosen the strength which best suits your condition.
Remember that it is important to take this medicine as your doctor has told you. The label should remind you how many puffs to take and how often. Check with your doctor or pharmacist if you are not sure.
This inhaler has a softer feel and a different taste than other inhalers you may have used before, because it is an extra fine aerosol which results in more of each dose being delivered to your lungs. Your doctor may prescribe a lower dose of this inhaler than your previously used beclometasone dipropionate inhaler. Even when your doctor has prescribed a lower dose, you may find that the number of puffs you are asked to take from this inhaler is the same as from your previous inhaler; this is because this inhaler may be a lower strength product (which means that each puff of this inhaler contains less beclometasone dipropionate than your old dipropionate inhaler).
DO NOT take more puffs than your doctor has told you
to. In some circumstances, your doctor may prescribe more than the usual number of puffs. You should check with your doctor or pharmacist if you are not sure. The usual number of puffs to take is:
Adults (including the elderly) and children over 12 years
• Mild to moderate Asthma
The starting dose is one puff twice a day. This may be increased to two puffs twice a day.
• Severe Asthma
The starting dose is two puffs twice a day. This may be increased up to four puffs twice a day.
The maximum dose is a total of eight puffs a day.
Children under 12 years
Qvar Autohaler is not recommended for use in children under 12 years.
What to do if you think your treatment is not working
If you think your usual treatment is not working, for example your symptoms are not getting better, or are getting worse, or you need to use more puffs from your reliever inhaler, or if your reliever inhaler does not seem to be working as well as usual, or your peak flow falls, please tell your doctor. Your asthma may be getting worse.
If you use more of your Qvar Autohaler than you should
It is important that you take your dose as stated on the pharmacist’s label, or as advised by your doctor. You should not increase or decrease your dose without seeking medical advice.
If you accidentally take more puffs than recommended, please tell your doctor.
If you forget to use Qvar Autohaler
If you forget to use this inhaler at your usual time, take your recommended number of puffs as soon as you remember unless it is nearly time to use your inhaler again. DO NOT take a double dose to make up for a forgotten dose. Then continue to use your inhaler regularly at the correct time, as prescribed by your doctor.
If you stop using Qvar Autohaler
This inhaler must be used regularly, even when you feel well. You must not stop using your inhaler unless your doctor tells you to.
Ask your doctor for a prescription for a replacement inhaler before this one is empty.
If your doctor decides to stop treatment, return the inhaler to your doctor or pharmacist for safe disposal.
Using your Qvar Autohaler device
Before using your inhaler, please read this leaflet carefully and follow the instructions. If you are not sure how to use the inhaler device, ask your doctor or a pharmacist.
Before use:
If this is a new device or if you have not used it for 2 weeks or more, it must be tested before use by releasing 2 puffs into the air in the following way:
1. Take the cover off from the mouthpiece, by pulling down on the lip at the back (fig. 1).
2. Point the mouthpiece away from you so that the puffs of medicine will go into the air. Push the lever up so that it stays up (fig.
2).
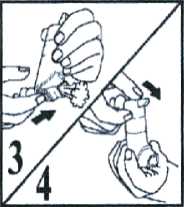
3. Then, to release a puff, push the dose release slide on the bottom of the device in the direction indicated by the arrow on it (fig. 3).
4. To release the second puff you need to return the lever to its down position (fig. 4) and follow steps 2 and 3 again. After releasing the second puff, return the lever to its down position, to be ready to take a puff of your medicine.
How to use your Qvar Autohaler device
Do not use the dose release slide to take your medicine; the Autohaler device will automatically release a dose when you begin to breathe in from the mouthpiece.
The instructions for taking a puff are given below.
1. Take the cover off from the mouthpiece, by pulling down on the lip at the back.
2. Hold your Autohaler device upright as shown. Push the lever up so that it stays up. Continue to hold your device upright, making sure that your hand is not blocking the air vent (marked by X in fig. 2) at the bottom of the device.
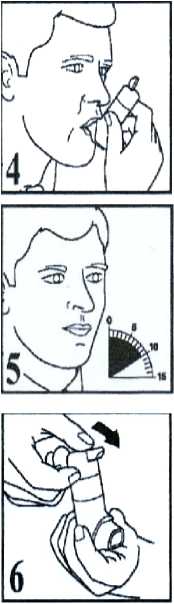
3. Breathe out as far as is comfortable, then immediately place the mouthpiece in your mouth, and close your lips around it.
4. Breathe in slowly and deeply through the mouthpiece. Do not stop breathing in when you hear the slight click and feel the puff in your mouth as it is important that you carry on breathing in after the puff is released.
5. Hold your breath for 10 seconds and then breathe out slowly.

6. The lever must be lowered to the down position after each puff. If your doctor has prescribed more than one puff, repeat steps 2-6. After use, replace the cover on the mouthpiece.
How to tell when your Qvar Autohaler device is empty
When the device is completely empty you will not feel or hear any propellant being discharged.
Cleaning instructions
For normal hygiene, the mouthpiece of your Autohaler device should be cleaned weekly with a clean, dry tissue or cloth. You should also rinse your mouth with water after using your inhaler.
Caution:
• Do not wash or put any part of your inhaler in water.
• Do not push a drying cloth or anything else into any part of the Autohaler device since it may cause damage to its operating parts
• Do not take the Autohaler device apart.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If immediately after taking a puff of this inhaler you feel wheezy or tight chested do not take any more puffs. Use your reliever inhaler to help your breathing and contact your doctor immediately.
Stop using your inhaler and tell your doctor immediately or go to the casualty department at your nearest hospital if the following happens:
• an allergic reaction (swelling of the lips, face or neck leading to severe difficulty in breathing; skin rash or hives).
This is a very serious but rare side effect. You may need urgent medical attention or hospitalisation.
Treatment with Qvar Autohaler devices may affect the normal production of corticosteroids in the body. Keep using your inhaler but see your doctor as soon as possible if you become unwell, particularly with any of the following:
• abdominal pain
• weakness
• vomiting
This is especially important if you have been exposed to other stress such as other illness, surgery or infection.
The following side effects may also occur in patients taking beclometasone dipropionate. If you experience any of these effects, keep using your inhaler but see your doctor if they last for a while or they are worrying you:
• hoarseness
• a sore mouth or thrush (white spots in your mouth and throat). These are less likely if you rinse your mouth out with water after using your inhaler. If you get thrush, your doctor may recommend a medicine to treat you
• feeling sick
• headache
• feeling dizzy or faint
• tremor
• change in taste
• increase in wheezing, shortness of breath and cough
• sleeping problems, depression or feeling worried, restless, nervous, over-excited or irritable. These effects are more likely to occur in children (Frequency not known).
At high doses, taken for prolonged periods the following side effects have been reported:
• bone thinning
• clouding of the lens of the eye (cataract) resulting in blurred vision
• loss of vision due to abnormally high pressure in the eye.
Children or adolescents who are using the inhaler for a prolonged period may grow more slowly. Your doctor may therefore wish to monitor the height of a child receiving prolonged treatment with Qvar Autohaler.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.qov.uk/vellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Qvar Autohaler
Do not store above 25°C. Protect from heat, light and frost.
KEEP OUT OF THE SIGHT AND REACH OF CHILDREN
If your device doesn’t appear to be working properly, becomes damaged or you notice any signs of deterioration, consult your pharmacist for advice.
The canister is pressurised and should not be punctured or burnt even if it seems empty. Do not use Qvar Autohaler after the expiry date that is stated on the outer packaging (shown as ‘EXP’). The expiry date refers to the last day of that month. Medicines should not be disposed via wastewater or household waste. If your doctor decides to stop treatment, return the inhaler to your doctor or pharmacist for safe disposal. These measures will help to protect the environment.
Leaflet revision date: 22nd March 2016
Qvar is a registered trademark of IVAX International GmbH.
Autohaler is a registered trademark of 3M Company.
PP6/1042/V2
6. Contents of the pack and other information
Qvar 100 Autohaler is a pressurised canister enclosed in a grey and part transparent autohaler actuator and metering device, part brick red body with a grey mouthpiece and grey cap.
Each actuation delivers 100 micrograms of the active ingredient beclometasone dipropionate into the mouth piece. Also contains Norflurane (HFA-134a) and ethanol.
What Qvar Autohaler looks like and contents of the pack:
• The Qvar Autohaler is a pressurised canister with a metering valve.
• Qvar 100 Autohaler is available in packs containing 200 actuations.
POM
PL 20774/1042 Qvar 100 Autohaler
Manufactured by 3M Health Care Limited, Loughborough, Leicester, United Kingdom. Procured from within the EU. Product Licence Holder: Quadrant Pharmaceuticals Ltd, Lynstock House, Lynstock Way, Lostock, Bolton, BL6 4SA. Repackaged by Maxearn Ltd, Bolton, BL6 4SA.
For further information about asthma, contact Asthma UK, the independent UK charity working to conquer asthma: Asthma UK, Summit House, 70 Wilson Street, London, EC2A 2DB. Asthma Helpline: 08457 010203 (Open Monday to Friday, 9am to 5pm. All calls charged at local rate).