Timolol Maleate 0.25% Ophthalmic Solution
PATIENT INFORMATION LEAFLET
GLAUCOL 0.25% & 0.5% EYE-DROPS
TIMOLOL MALEATE
PLEASE READ THIS LEAFLET CAREFULLY BEFORE YOU START TAKING THIS MEDICINE.
KEEP THIS LEAFLET UNTIL YOU HAVE FINISHED ALL THE PRESCRIBED COURSE OF GLAUCOL.
IF YOU HAVE ANY QUESTIONS CONCERNING YOUR MEDICINE ASK YOUR DOCTOR OR PHARMACIST FOR MORE INFORMATION.
What is in your medicine?
Glaucol eye-drops contain the active ingredient Timolol Maleate BP along with the inactive ingredients sodium chloride, sodium hydroxide and water.
Glaucol eye-drops come in two strengths: 0.25% w/v & 0.5% w/v.
Both strengths come in cartons of 30 vials, and both strengths are clear bright colourless and odourless liquids.
The manufacturer of Glaucol is:
Steripak Ltd.,
Goddard Road, Astmoor, Runcorn,
Cheshire WA7 1QE
The Product Licence Holder is:
Chelonia Healthcare Limited,
Boumpoulinas 11, 3rd Floor,
Nicosia, P.C. 1060, Cyprus
How does Glaucol work?
Timolol Maleate belongs to a group of chemicals known as beta- blockers. It is thought Timolol Maleate works by reducing the amount of liquid humor in the eyeball causing an overall reduction in pressure.
Why have you been prescribed Glaucol eye- drops?
You have been prescribed Glaucol eye-drops to lower the pressure in your eyeballs. There are a number of causes of raised eyeball pressure, glaucoma being a common one.
If you are not sure why you have been prescribed Glaucol, then please ask your doctor.
Before you use Glaucol eye-drops.
Before taking this medicine, tell your doctor if you have ever had any unusual or allergic reactions to Glaucol, other beta- blocker medicines or any of the other ingredients of this medicine. Also tell your doctor about any other allergies, i.e. foods, dyes, preservatives.
Do not use Glaucol eye-drops if:
• You are allergic to timolol maleate, beta-blockers or any of the other ingredients
• You have now or have had in the past breathing problems such as asthma, chronic obstructive pulmonary disease (severe lung disease which may cause wheeziness, difficulty in breathing and/or long-standing cough)
Take special care with Glaucol eye-drops:
Before you use this medicine, tell your doctor if you have now or have ever had in the past:
• coronary heart disease (symptoms of which include chest pain or tightness, breathlessness or choking), heart failure, low blood pressure (hypotension)
• disturbances of heart rate such as a slow heart beat (bradycardia)
• poor blood circulation disease (peripheral arterial disease) such as Raynaud's disease or Raynaud's syndrome
• diabetes as timolol may mask the signs and symptoms of low blood sugar • overactivity of the thyroid gland as timolol may mask the signs and symptoms
Paediatric population. Timolol eye drop solution should generally be used with caution in young patients. In newborns, infants and younger children Timolol should be used with extreme caution. If coughing, wheezing, abnormal breathing or abnormal pauses in breathing (apnoea) occur; the use of the medication should be stopped immediately. Contact your doctor as soon as possible. A portable
apnoea monitor may also be helpful.
Timolol Maleate eye-drops have been studied in infants and children aged 12 days to 5 years, who have raised pressure in the eye(s) or have been diagnosed with glaucoma.
For more information, talk to your doctor
Use in pregnancy and while breast-feeding
Do not use Glaucol eye-drops if you are pregnant, unless your doctor considers it necessary.
Do not use Glaucol eye-drops if you are breast-feeding. Timolol may get into your milk. Ask your doctor for advice before taking any medicine during breast-feeding.
Can you drive when taking Glaucol?
This medicine can cause temporary blurring of the vision. After administering the eye-drops wait for any blurring of the vision to subside before you drive or operate machinery.
Can you take Glaucol with other medicines?
Glaucol can affect or be affected by other medicines you are using. Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including those medicines obtained without a prescription.
Tell your doctor if you are using or intending to use any of the following medicines which can interfere with Timolol.
• Medicines to treat high blood pressure
• Medicines to treat certain heart conditions
• Other eye-drops for the treatment of glaucoma
• Medicines for diabetes
• Quinidine, used to treat heart conditions and some types of malaria
• Antidepressants known as fluoxetine and paroxetine
If you are taking any of the above speak to your doctor before taking this medicine.
Tell your doctor before you have an operation that you are using Glaucol eye-drops as timolol may change the effects of some medicines used during anaesthesia.
When to take Glaucol eye-drops
Always use Glaucol eye-drops exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure. These eye-drops should only be applied externally to the eyes and only in the doses prescribed by your doctor. Do not take more of it, and do not take it more often or for a longer time than your doctor ordered.
Usual doses are stated below.
Recommended therapy is one drop 0.25% solution in the affected eye(s) twice a day.
If the patient doesn't respond the dose is increased to 0.5% solution.
Your doctor will assess the correct dosage for you if you are transferring from another medicine.
Glaucol eye-drops come in uni-dose vials. there is only enough for one dose in each vial.
How to apply the eye-drops
Wash your hands before applying the eye-drops. Break seal on vial so it's ready for use.
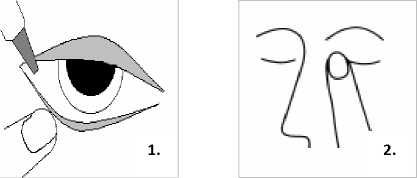
Tilt your head backwards and using your fingers pull your eye lids far apart. Gently squeeze the contents of the vial directly onto your eyeball, (picture 1). After using Glaucol eye-drops, press a finger into the corner of your eye, by the nose (picture 2) for 2 minutes. This helps to stop Timolol getting into the rest of the body.
Paediatric population. A detailed medical examination should precede the use of Timolol. Your doctor will carefully evaluate the risks and benefits when considering treatment with Timolol. If the benefits outweigh the risks, it is recommended to use the lowest active agent concentration available once daily. With regard to "the use in children", the 0, 1% active agent concentration may be sufficient to control pressure within the eye. If the pressure is not sufficiently controlled with this dosage, a twice daily application at 12-hourly intervals may be necessary. Patients, especially newborn, should be closely observed for one to two hours after the first dose and careful monitoring for adverse events should be carried out until surgery is performed.
One drop only of Timolol should be instilled per dosing time. After instillation keep the eyes closed for as long as possible (e.g. 3 - 5 minutes) and apply pressure to the corner of the eye closest to the nose to prevent Timolol eye drops spreading throughout the body.
Duration of treatment. For a transient treatment in the paediatric population.
What to do if you take too much of your medicine at the same time
It is unusual to be able to overdose on Timolol Maleate by just applying it externally to the eyes. If it is accidentally drunk contact your nearest doctor or hospital casualty department at once. Take any remaining vials with you and keep them in the original container or packaging so that they can be identified
What if you miss a dose?
If you miss a dose, skip the missed dose and go back to your regular dosage schedule. Do not double the dose.
You may not feel any different taking Glaucol eye-drops, but the drops are helping to reduce your eyeball pressure and you should continue with your medication until your doctor says you no longer need it.
What side effects can Glaucol cause?
Like all medicines Glaucol eye-drops can cause side effects although not everyone gets them.
You can usually carry on taking the drops, unless the effects are serious. If you are worried, talk to a doctor or pharmacist.
Like other medicines applied to the eyes (topically applied ophthalmic drugs), Timolol is absorbed into the blood. This may cause
similar side effects as seen with systemic beta-blocking agents. Side effects after topical application into the eyes are lower than
when medicines are, for example, taken by mouth or injected. Listed side effects include reactions seen within the class of beta-
blockers when used for treating eye conditions;
• allergic reactions including sudden swelling of the face, lips mouth, tongue or throat which may cause difficulty swallowing or breathing (angioedema), hives (urticaria), localised and generalised rash, itchiness (pruritus), sudden life-threatening allergic reaction (anaphylactic reaction)
• low sugar levels in the blood (hypoglycaemia)
• difficulty sleeping (insomnia), depression, nightmares, memory loss
• fainting (syncope), stroke (cerebrovascular accident), decreased blood flow to parts of the brain (cerebral ischemia), increases in signs and symptoms of myasthenia gravis (muscle disorder), dizziness, tingling or numbness of hands and feet, pins and needles (paraesthesia), headache
• signs and symptoms of eye irritation (e.g. burning, stinging itching, tearing, redness), swollen eyelid (blepharitis), irritation or feeling of having something in the eye (keratitis), blurred vision and low eye pressure and visual disturbances after an eye operation (choroid detachment following filtration surgery), decreased corneal sensitivity, dry eyes, damage to the front layer of the eyeball (corneal erosion), drooping of the upper or lower eyelid (ptosis), double-vision (diplopia)
• slow heart beat (bradycardia), chest pain, palpitations, fluid build-up (oedema), changes in the rhythm or speed of the heart beat (arrhythmia), heart disease with shortness of breath and swelling of the feet and legs due to fluid build up (congestive heart failure), heart condition (atrioventricular block), heart attack (cardiac arrest), heart (cardiac) failure
• low blood pressure (hypotension), poor blood circulation which makes the toes and fingers numb and change colour (Raynaud's phenomenon), cold hands and feet
• bronchospasm (wheezing or difficulty breathing - usually in patients with pre-existing bronchospastic disease), shortness of breath (dyspnoea), cough
• taste disturbances (dysgeusia), nausea, indigestion (dyspepsia), diarrhoea, dry mouth, abdominal pain, vomiting
• hair loss (alopecia), skin rash with white silvery coloured appearance (psoriasiform rash) or worsening of psoriasis, skin rash
• muscle weakness or pain not caused by exercise (myalgia)
• sexual dysfunction, decreased libido
• unusual muscle weakness or pain not caused by exercise (asthenia) or tiredness (fatigue)
If any of the side effects get serious, or if notice side effects not mentioned in this leaflet, please tell your doctor or pharmacist.
Storing your medicine
You must keep this medicine in a safe place where children cannot get hold of it. Your medicine could harm them.
Store below 25°C, away from light. Keep cartons securely closed. Keep the vials in the containers in which they were given to you.
On the label you will find the words "Expiry Date" followed by numbers indicating the day, month and year. This is the date when the medicine is no longer fit for use. Do not use Glaucol after this date, but return it to your doctor or pharmacist.
A reminder
REMEMBER this medicine is for you. Never give it to someone else, even if their symptoms are the same as yours.
This leaflet does not contain the complete information about your medicine. If you have any questions or are not sure about anything, ask your doctor or pharmacist who have access to additional information.
This leaflet was revised in December 2011